How to Prevent the Leading Cause of Blindness i.e. Trachoma from the World?
Trachoma, earlier known as Egyptian ophthalmia means rough in the Greek language. In this condition, the cornea becomes rough in later stages when it becomes chronic. It is one of the causes of preventable blindness in the whole world.
Trachoma disease is a chronic keratoconjunctivitis that mainly affects the superficial epithelium of the cornea and conjunctiva simultaneously. It is characterized by a mixed follicular and papillary response of conjunctival tissue, pannus formation, and in late stages, cicatrization giving a rough appearance.
Etiology
- Causative organism: Trachoma is caused by the bacterium Chlamydia trachomatis. There are many serovars of Chlamydia trachomatis. At present, there are 12 serovars, namely A, B, Ba, C, D, E, F, G, H, I, J, and K.
- Predisposing factors:
- Age: It mainly occurs in infancy and early childhood
- Sex: It is more common in females
- Race: No one is immune to trachoma
- Climate: It is majorly seen in dry and dusty weather
- Socioeconomic status: This disease is more common in people who live in unhygienic conditions, overcrowded places and unsanitary conditions, abundant fly population, paucity of water, and lack of materials like no separate towels, and no separate handkerchiefs. Another major factor is the lack of education and the people are also not aware of the spread of the contagious disease (diseases that are spread by touch).
- Environmental factors: These include smoke, sunlight, irritants, and exposure to dust. All these factors increase the risk of disease and due to this reason, outdoor workers are more affected as compared to office workers.
- Source of infection: The major source of infection in the trachoma endemic zone is the discharge of the conjunctiva of the affected person.
- Infection mode: It may spread from one eye to another eye by any of the following modes:
1 . Direct spread of infection can occur through contact by airborne or water-borne modes.
2. Vector transmission of trachoma is mainly common through flies.
3. Material transfer plays a major role in the spread of the disease. This can occur through contaminated fingers of nurses, doctors, and tonometers. It also includes the use of common handkerchiefs, towels, Surma rods, and bedding.
This disease spread worldwide but it is mainly prevalent in certain regions like North Africa, the Middle East, and certain regions of Southern Asia. This disease is mainly responsible for the world’s blindness second only to cataracts.
Clinical and pathological features
Clinical features can be described into two phases:
- Phase of active inflammatory trachoma
This occurs during childhood due to active infection of Chlamydia. The incubation period varies from one week to 2 weeks. The disease has an insidious onset and it can be present in acute form but rarely. The trachoma signs and symptoms are mentioned below:
Symptoms:
Symptoms are determined based on the presence or absence of any other secondary bacterial infection.
In the presence of secondary bacterial infection, the symptoms are:
- Discomfort
- Foreign body sensation
- Grittiness
- Blurring
- Redness of eyes
If secondary bacterial infection is absent, the symptoms are :
- Mild foreign body sensation
- Occasional lacrimation
- Slight stickiness of the lids
- Scanty mucoid discharges
Other symptoms are mild photophobia, discharge from the eyelids making them stick together during sleep, slight blurring of vision, and colored halos may be complained by some of the patients because of the mucus present on a cornea having a prismatic effect.
Signs:
Conjunctival signs:
These are seen in upper tarsal and forniceal conjunctiva congestion.
- Conjunctival follicles: In this case, follicles look like boiled sago grains. These are more commonly seen on upper tarsal conjunctiva and fornices but may also be present on the lower fornix, plica semilunaris, and caruncle. Sometimes follicles may be seen on the bulbar conjunctiva, and these are the pathognomic of the disease trachoma.
Pathologically, follicles are formed due to the scattered aggregation of other cells and mainly lymphocytes in the layer of the adenoid. Each follicle has a central part which is made up of mono-nuclear histiocytes, few lymphocytes, and large multi-nucleated cells known as Leber cells. It is also having a cortical part that is made up of lymphocytes showing active proliferation and blood vessels are present in most peripheral parts. In later stages, signs of necrosis can also be seen. So, there is the presence of Leber cells and signs of necrosis which differentiate the trachoma follicles from other follicles of follicular conjunctivitis.
- Papillary hyperplasia: Papillae can be defined as flat-topped raised reddish areas in which the tarsal conjunctiva has a red and velvety appearance. Pathologically, each papillae consist of the central core of numerous dilated blood vessels surrounded by lymphocytes and covered by epithelium that is hypertrophied.
Corneal signs:
- Superficial keratitis may be present in the upper part of the cornea.
- Herbert follicles referred to as typical follicles are present in the limbal area. Histologically, these are similar to conjunctival follicles.
- Progressive Pannus referred to as infiltration of the cornea associated with vascularization is seen in the upper part. The vessels are superficial and lie between the epithelium and the bowman’s membrane. Later on, the bowman’s membrane is also destroyed. A corneal ulcer may develop at the advancing edge of the Pannus. Usually, such ulcers are shallow and may become chronic.
- Phase of Chronic Cicatricial Trachoma
It occurs in middle age and results due to continued mild-grade chronic inflammation. It consists of a type 4 hypersensitivity reaction due to the intermittent present antigens of Chlamydia that are responsible for this phase of trachoma. This stage is also referred to as the sequelae of trachoma. The phase has the following clinical features:
Conjunctival signs:
- conjunctival scarring may be irregular, star-shaped, or linear. There is the presence of a linear scar in the sulcus subtarsalis which is known as Arlt’s line.
- Concretions are also present that look like hard whitish deposits vary in size. They are not deposits of calcium. They are usually formed due to the collection of dead epithelial cells and mucus in the depression called glands of Henle.
- The other sequelae include xerosis, pseudocyst,
Corneal signs:
- Regressive pannus in which the vessels extend a short distance beyond the infiltration area.
- Herbert pits are circular or oval pitted scars left after healing of the follicles of Herbert in the limbal area.
- Corneal ectasia, xerosis of the cornea, and total corneal pannus are the corneal sequelae.
Lid signs:
- Ptosis (drooping upper eyelid)
- Madarosis (loss of eyebrows or eyelashes)
- Trichiasis (misalignment of eyelashes)
- Entropion (eyelids turn inwards)
- Tylosis (thickening of the tarsal border of the eyelid)
- Ankyloblepharon (adhesion of upper and lower eyelids)
Lacrimal apparatus signs:
- Chronic dacryocystitis
- Chronic dacryoadenitis
Grading of Trachoma
WHO grading system classifies trachoma into 5 grades. Grading of trachoma is done according to FISTO classification as follows:
F: Trachomatous Inflammation Follicular
I: Trachomatous Inflammation Intense
S: Trachomatous Scarring
T: Trachomatous Trichiasis
O: Corneal Opacity
Complications
Corneal ulcer
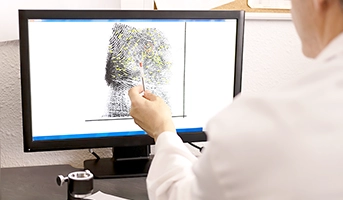
Diagnosis of Trachoma
- Clinical diagnosis – Done from its clinical signs and symptoms
- Laboratory diagnosis:
- Conjunctival cytology
- Detection of inclusion bodies
- ELISA
- PCR
- Isolation of Chlamydia
- Serotyping of TRIC agents
Management of Trachoma
- Treatment of Active Inflammatory Trachoma
- Antibiotic therapy is the mainstay of treatment.
- Topical antibiotics are less effective than the systemic antibiotics.
- Azithromycin as a single oral dose is the treatment of choice.
- Erythromycin is an alternative single oral dose for women at child bearing age.
- Doxycycline and oral tetracycline are contraindicated in children below 8 years, during pregnancy, and breastfeeding.
- Treatment of Inactive Trachoma
- In this case, artificial tears such as 1% person carboxymethyl cellulose may be added for a soothing effect.
- Surgical therapy can be considered for:
- Conjunctival Sequelae: Concretions removed with the help of a hypodermic needle. Conjunctival xerosis should be treated by lubricating drops.
- Eyelid Sequelae: Trichiasis treated by electrolysis, cryolysis, and radio frequency epilation. Entropion is treated surgically.
- Corneal Scarring: Penetrating keratoplasty and keratoplasty.
Prophylaxis for trachoma infection and blindness
WHO has adopted a strategy for the prophylaxis for trachoma i.e., SAFE Trachoma Strategy, where:
S – SURGERY (Tertiary prevention)
- Bilamellar tarsal rotational surgery at a community for all the affected persons.
A – ANTIBIOTICS (Secondary prevention)
- Oral Azithromycin administration to all community members in areas with 10% or more prevalence.
- Tetracycline eye ointment for all pregnant women and all others allergic to macrolides.
F – FACIAL HYGIENE (Primary prevention)
- Frequent face wash
- Common use of the handkerchief, towel, and Surma rods should be avoided.
E – ENVIRONMENTAL CHANGES (Primordial prevention)
- Refuse dumps
- Provision of water latrines and good water supply to reduce flies
- Sprays to control flies
- Health education to improve personal and environmental hygiene.
To get conceptual clarity on the MBBS courses online, click here.
FREQUENTLY ASKED QUESTIONS (FAQs)
Q.1 What do you mean by madarosis and tylosis?
Answer: Madarosis is the absence or loss of eyelashes either due to infection or congenital and tylosis is a thickening of lid margins.
Q.2 What is trichiasis?
Answer: Trichiasis is referred to as the ingrowth of eyelashes.
Q.3 Why does corneal ulcer occur as a complication of trachoma?
Answer: It may occur due to rubbing by concretion, or trichiasis with a superimposed bacterial infection.
Q.4 What do we call the intracytoplasmic inclusion bodies of Chlamydia trachomatis?
Answer: HP bodies (Halberstaedter Prowazek bodies) are the intracytoplasmic inclusion bodies of Chlamydia trachomatis.
Related post