What is Parkinson’s Disease? A Deep Dive for Medical Students
We will take a deep dive into Parkinson’s disease in this blog, covering everything from its fundamentals to clinical symptoms, classifications, clinical diagnosis, risk factors, and potential therapies.
What is Parkinson’s disease?
In 1817, Parkinson’s disease was initially described by Dr. James Parkinson as “shaking Palsy”. Parkinson’s disease is one of the most common neurological conditions and affects around 1% of people over the age of 60 years. It is a progressive, chronic neurodegenerative disorder that causes both motor and non-motor symptoms.
This neurological condition has clinical effects on patients, families, and caregivers due to its degenerative impact on movement or slow movement and stiff muscle control. The death of striatal dopaminergic neurons is responsible for motor symptoms of Parkinson’s disease, but the presence of non-motor symptoms also suggests neuronal loss in non-dopaminergic sites.
The term parkinsonism describes a group of clinical symptoms that are considered cardinal signs related to motor function or clinical features of Parkinson’s disease, including bradykinesia, resting tremor, and muscle stiffness.
The condition Parkinson disease is associated with Lewy bodies and degeneration of dopaminergic neurons in the substantia Nigra. For normal movements, brain cells require dopamine which sends activation signals for fine-tune movements, due to lack in dopamine levels it causes slowness of movements. Though it develops gradually, the condition is progressive.
Frequent tremors could potentially link to rigidity and bradykinesia are initial common clinical symptoms of PD. One of the major negative influences of Parkinson’s disease is Postural instability and involuntary movements which affect the quality of life and usually occur in later stages of the disease.
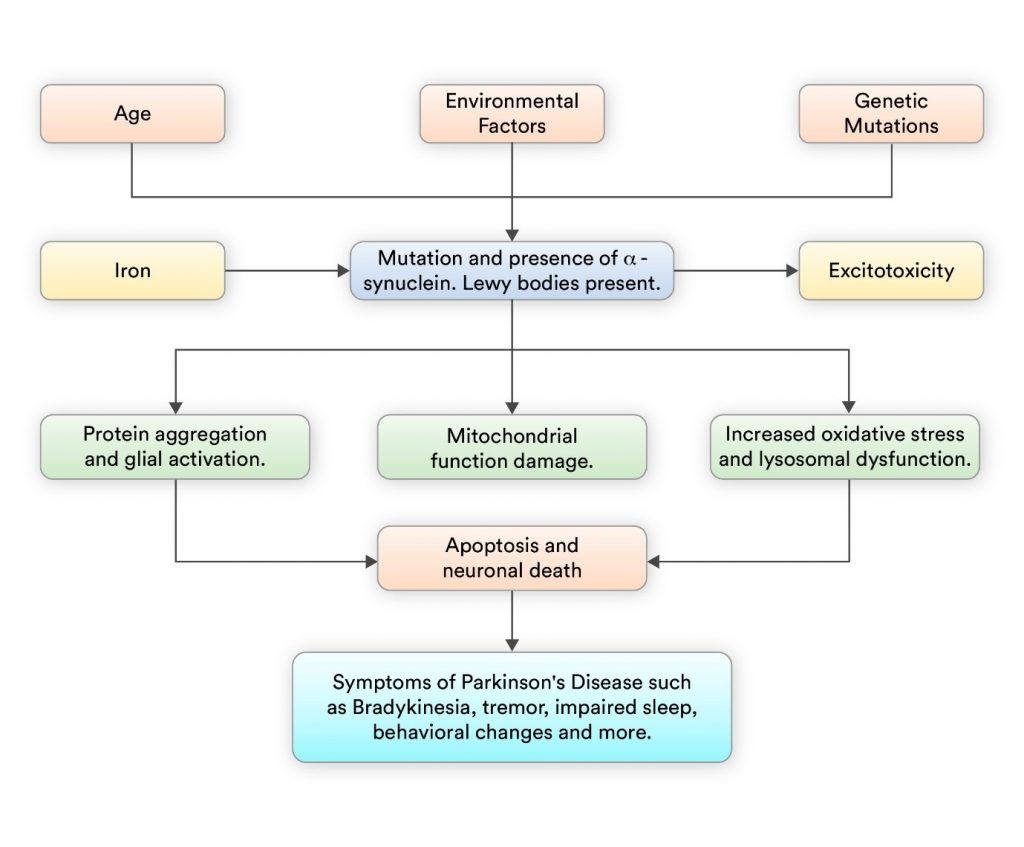
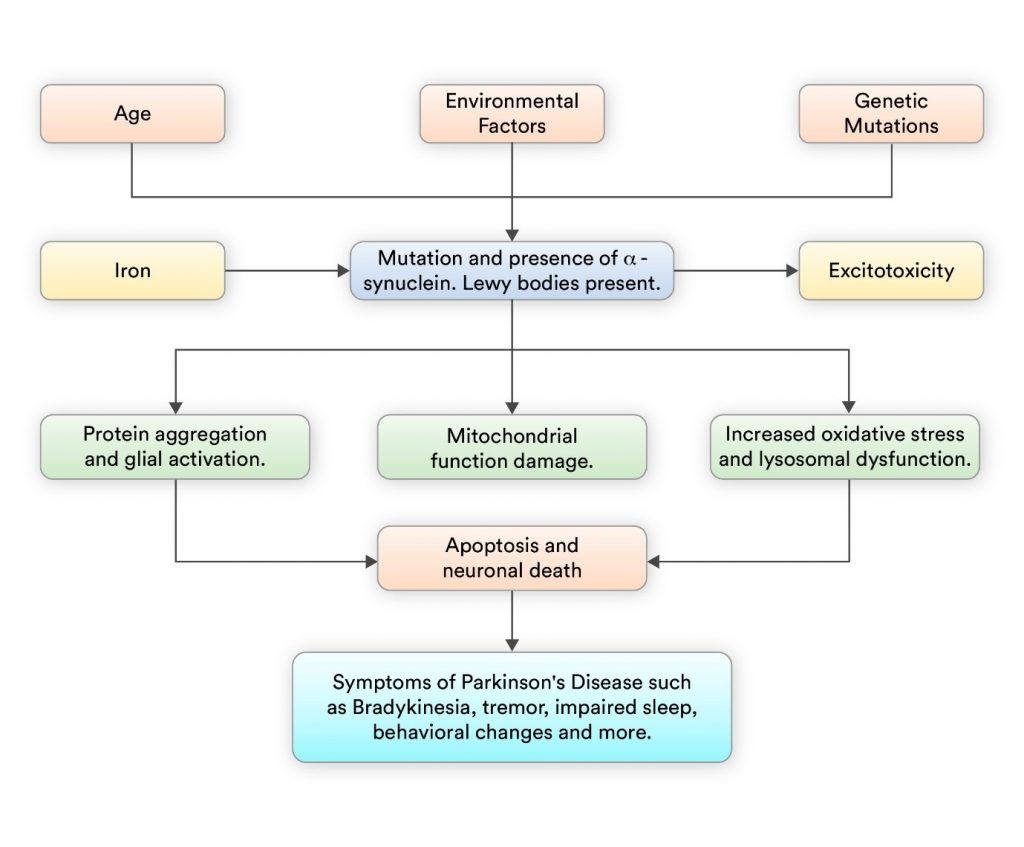
What is the pathophysiology of Parkinson’s Disease?
The pathophysiology of PD involves a combination includes a combination of environmental factors, toxins, genetic mutations, and mitochondrial dysfunction leading to neurodegeneration. The key factors involve the formation of Lewy neurites, impaired protein degradation, and the progressive loss of dopamine neurons in the brain’s substantia nigra. Understanding this mechanism is important for developing effective symptomatic treatment to slow the disease progression.
What are the warning signs and symptoms of Parkinson’s disease?
- Primary Parkinson’s Disease Symptoms
- Parkinson’s disease is characterized by tremor, which typically starts in the hand and affect the foot or jaw in the initial phase. This tremor exhibits a rhythmic back-and-forth motion action involving the thumb and fingers, like pill-rolling. Tremor typically diminishes during sleep, but visible when the hand is at rest or under stress.
- Most patients with Parkinson’s disease have muscle rigidity which is characterized by muscle stiffness or resistance in movement. This stiffness and or resistive movement results in restricted mobility. In this, the affected person’s arm exhibits jerky movements known as ‘cogwheel’ stiffness.
- Bradykinesia refers to a movement disorder that results in slowness of movement for both spontaneous and automatic movements, which affects daily living activities. Even simple activities take a lot of effort such as washing or dressing, which may not require lots of time and effort. Furthermore, patients with bradykinesia exhibit a reduction in facial expression, commonly known as ‘masked face’.
- Postural instability and involuntary movements present as changes in posture and poor balance which results in increasing falls.
- In children, speech may be lacking or rapid, and slurring of words or hesitancy before speaking are usual signs of Parkinson’s disease and it also includes difficulty in writing small words.
- Motor symptoms related to Parkinson’s disease:
-
- Slowed Movement
- Tremor while the muscle is at rest
- Stiffness or Rigidity
- Walking gait and Unstable posture
- Reduced control of facial muscles or features
- Drooling due to loss of facial muscle control or swallowing dysfunction
- Non-motor symptoms related to Parkinson’s disease:
-
- Appear at the earliest stage of disease
- Autonomic nervous system symptoms: Dry mouth, Urinary incontinence, orthostatic hypotension, mental health disorders such as depression, and sexual dysfunction.
Non-motor symptoms may include a wide range of psychological symptoms sleep disorder, impulse control disorder, or behavior disorder which includes rapid eye movements or restless legs syndrome.
What are the stages of Parkinson’s disease?
There are five stages to explain the progress of PD which is characterized by different symptoms and challenges. These stages vary from person to person, and there are generally five main stages:
Early Stage (Stage 1)
- Tremor or other movement may be present on the side of the body.
- Change in posture and facial expressions.
Stage 2 (Moderate Parkinson’s Disease)
- In the moderate stage, may affect both sides of the body.
- Tremor, stiffness, and slowness of movement worsen.
- Balance and walking become more difficult.
Stage 3 (Mid-Stage Parkinson’s Disease)
- Difficult to maintain balance and coordination.
- Daily living activities become more challenging or may need assistance.
Stage 4 (Advanced Parkinson’s Disease)
- Movement may be severely impaired, and walking and standing may be difficult without assistance.
- Tremors and rigidity are present, and assistance is often required.
Stage 5 (Parkinson’s Disease with End-Stage Complications)
- This is a severe stage of Parkinson’s disease. Individuals may be unable to walk or stand or may be bedridden/wheelchair bound.
- Cognitive and psychiatric symptoms may present such as dementia or hallucinations.
- Difficulty in swallowing or severe complications such as infections may occur.
What are the different clinical features of Parkinson’s disease?
Parkinson’s disease is commonly divided into many categories, each with the type of characteristics and manifestations. The following are some different types of Parkinson’s disease:
- Idiopathic Parkinson’s disease: This is the most common type of Parkinson’s disease with no recognized etiology. It typically represents motor symptoms like tremors, bradykinesia, postural instability, and rigidity.
- Parkinsonism: It is a group of neurologic disorders that share similar characteristics with Parkinson’s disease, but the causes are different.
Examples include:
-
- Drug-induced Parkinsonism: Caused by certain medications, such as antipsychotics or antiemetics.
- Vascular Parkinsonism: Caused by reduced blood flow to the brain, often due to small strokes or cerebrovascular disease.
- Atypical Parkinsonism includes another different type of neurologic disorders with Parkinson like common symptoms of Progressive Supranuclear Palsy (PSP), Corticobasal Degeneration (CBD), and Multiple System Atrophy (MSA).
- Young-onset Parkinson’s disease: PD occurs before the age of 50, it is referred to as young-onset. In young-onset Parkinson’s disease, may progress differently than typical PD and can present with various difficulties.
- Secondary Parkinsonism: This type of Parkinson’s disease includes other conditions or factors, such as encephalitis, traumatic brain injury, or exposure to toxins.
- Genetic types of Parkinson’s disease: Parkinson’s disease can have a genetic factor. Certainly, gene abnormalities are associated with an increased chance that the condition may occur. Most Parkinson disease cases are sporadic with no genetic cause, but genetics play a role in some cases.
- In some cases, Parkinson disease can have a genetic component. Certain gene mutations are associated with an increased risk of developing Parkinson’s, and familial forms of the disease may occur. While genetics play a role in some cases, most Parkinson’s cases are sporadic, with no known genetic cause.
What is Parkinson’s disease differential diagnosis and early detection?
A clinical approach is involved to diagnose Parkinson disease, in which a physical examination is to check the presence and absence of Parkinson disease signs & symptoms through patient online or offline interviews with a detailed neurological examination.
- During the physical examination:
-
- Cognitive skills are evaluated.
- Facial expressions are observed for abnormalities.
- Tremors in the face, hands, arms, or legs are noted.
- Presence of muscle rigidity or stiffness in the arms, legs, torso, or shoulders is assessed.
- Ability to rise from a chair without using arms is tested.
- Walking patterns and balance while standing are analyzed.
- Additionally, neuroimaging techniques may be utilized:
-
- Magnetic resonance imaging (MRI) examines the brain’s structure.
- DaTscan, an FDA-approved imaging test, detects dopamine function in the brain, aiding in distinguishing idiopathic Parkinson disease from other neurologic disorders. Uncertain Parkinsonism
Note: In the early stages of Parkinson’s disease, a comprehensive evaluation by a movement disorder specialist is important.
Differential Diagnosis:
Differential diagnosis depends on careful history, physical examination, progression of the disease, and symptomatic treatment.
- Secondary Parkinsonism includes multiple causes of parkinsonism which can differentiated through appropriate imaging, history, and physical examination.
- Lew body dementia includes motor symptoms with early onset of hallucinations and cognitive dysfunction which precede motor symptoms.
- Vascular parkinsonism includes Parkinson’s disease symptoms with vascular events such as cerebral stroke. Damage to the dopaminergic pathways can cause vascular parkinsonism and similar symptoms.
What are the main risk factors of Parkinson’s disease?
Parkinson’s disease risk factors include:
- Age: Parkinson’s disease is uncommon in young adults, typically emerging in middle to late life, with the risk escalating with age. Young onset commonly occurs before 60 or older, while it is rare in younger people. Younger individuals with Parkinson disease may have different work, social and pharmaceutical side effects, therefore further precautions are needed.
- Heredity: Having a close family member with Parkinson’s disease heightens the likelihood of developing the condition. However, the risk remains relatively low unless several family members have Parkinson’s disease.
- Sex: Men exhibit a higher propensity for developing Parkinson’s disease compared to women.
- Post-traumatic brain injury: Head injuries increase the risk of Parkinson’s disease.
What are the various effective treatment approaches for Parkinson’s disease?
- Medication Management: Most Parkinson’s disease patients ultimately require medication to alleviate their motor symptoms. There are different drug classes are accessible for the treatment. The most effective and primary symptomatic therapy is Carbidopa/Levodopa as an add-on treatment with numerous strengths and formulations. It is frequently administered alongside other medication classes such as Catechol-O-Methyltransferase (COMT) Inhibitors, Dopamine Agonists, Monoamine Oxidase-B Inhibitors (MAO), and Anticholinergic agents. Dopamine agonists and enzyme inhibitors stimulate the production of dopamine in the brain which reduces involuntary movements. These drug therapy treatment plans are highly personalized for the patient and are modified over time in response to possible adverse effects and potential side effects. Scientists are exploring other ways to identify biomarkers for PD to slow down the disease process with more tailored treatment and for earlier diagnosis.
- Surgical Treatment:
Deep Brain Stimulation (DBS):
-
- A surgical procedure approved by the FDA for over a decade. In deep brain stimulation procedure, it generates electrical pulses and sends them to the brain which may reduce Parkinson’s disease symptoms.
- Neural stimulation in PD treatment involves four areas of the brain which are globus pallidus interna, thalamus, subthalamic nucleus, and pedunculopontine nucleus. DBS of the thalamic improves tremor while DBS of the globus pallidus interna improves motor function.
- The insertion of an electrode into a specific brain region, typically the globus pallidus interna (GPI) or subthalamic nucleus (STN).
- Implants can be placed unilaterally or bilaterally as necessary.
- The pacemaker-like device is linked with electrodes beneath the skin in the chest.
- Suitable candidates demonstrate a robust response to Levodopa, without significant cognitive or psychiatric impairments, and minimal balance issues.
- Benefits include alleviating medication-resistant tremors and managing motor fluctuations, such as dyskinesia, throughout the day.
- Deep brain stimulation is primarily recommended for individuals with advanced Parkinson’s disease who experience motor fluctuations and medication-resistant symptoms. However, DBS does not cure Parkinson’s disease but can help alleviate certain motor symptoms. DBS can be an effective treatment for treating the Subthalamic nucleus or globus pallidus interna with primary motor symptoms as clinical features in Parkinson’s disease.
What is the different therapy approaches for Parkinson’s disease?
There are different therapy approaches for PD which include physical therapy, occupational therapy, rehabilitation therapy for lifestyle modifications, and help in daily living activities:
Physical Therapy:
-
- Physical therapy mainly focuses on improving range of motion, muscle strength, balance, or overall physical mobility in people with PD.
- With physical therapy, the exercises and activities help to address specific motor symptoms such as gait disturbances and muscle rigidity.
Occupational Therapy:
-
- Occupational therapy mainly focuses on the patient’s activities of daily living (ADLs) to enhance and maintain independence.
- Occupational therapists provide a strategic approach for patients to overcome challenges related to fine motor skills, gross motor skills, or self-care tasks.
- Assistive modalities may also be recommended to support functional independence at home and in the community.
Rehabilitation Therapy:
-
- Regular exercise has been shown to have numerous benefits for individuals with Parkinson’s disease. It can improve balance, flexibility, and muscle strength, as well as enhance overall quality of life.
- Speech therapy or voice exercises can help individuals overcome speech difficulties, such as soft speech or slurred speech.
- Eating a healthy diet rich in fruits, vegetables, whole grains, and lean proteins may help manage symptoms and improve overall well-being.
- Support from family, friends, and support groups can provide emotional and practical support and reduce feelings of isolation.
Multidisciplinary Care for Parkinson’s disease:
-
- A comprehensive approach involving various healthcare professionals such as rehabilitation specialists, neurologists, nurses, social workers, and other providers.
- Recommended for addressing the multifaceted needs of Parkinson’s disease (PD) patients effectively.
- Collaboration ensures customized treatment plans that are coordinated across different aspects of care.
Parkinsonism is a complex and evolving field, to stay informed about the latest developments or for new advances in treatment plans, don’t forget to read the most recent books, and articles and go to conferences or seminars on the subject will contribute to your effectiveness as a future health care professional.
Frequently Asked Questions (FAQs):
Q1. What are the latest advancements in Parkinson’s disease treatment?
Ans. Focused ultrasound thalamotomy is a non-invasive treatment approach for tremors in which ultrasound waves create a lesion in a specific area of the brain called the thalamus. It has shown visible results in reducing tremors in people with Parkinson’s disease.
Q2. How to differentiate between Parkinson’s disease from Vascular parkinsonism?
Ans. Parkinson’s is caused by gradual loss of nerve cells, and it is not progressive whereas vascular parkinsonism is caused by one or more small strokes.
Q3. What is the novel biomarker for Parkinson’s disease?
Ans. There are several novel biomarkers for Parkinson’s disease that are under investigation, but the one promising biomarker is alpha-synuclein, a protein found in Lewy bodies that is closely linked to the pathology of PD.
Related post