Becoming a specialist physician is a long, challenging but fruitful journey. Amid this journey, crossing the milestone of (Membership of the Royal Colleges of Physicians) MRCP Part 1 exam is highly crucial. To help you with details, we are here with the blog covering ‘MRCP PART 1 Exam Dates 2024.’ Here, we’ll dive deep into the specifics, studying a comprehensive guide with great insights.
What is MRCP Part 1?
The MRCP exam puts a medical student’s knowledge and skills to the test. It is a challenging exam that evaluates basic concepts not only from roots but also the practical knowledge overall. It assesses knowledge and understanding of medical sciences and the ability of a candidate to apply the knowledge in real-world situations. It is merely not an exam, it’s a pathway for the candidates who wish to specialize in medicine.
What Does MRCP Offers?
MRCP offers masters/postgraduate level medical diploma in internal medicine in the UK. It holds importance and value as it is globally recognised. It is acknowledged in the countries overall, with some being UK, UAE, Ireland, Singapore, etc. An MRCP qualified medical student/candidate can have many location options to continue medical practice. For the doctors who are preparing for specialization on the behalf of the Royal College of Physicians of Edinburgh, the Royal College of Physicians and Surgeons of Glasgow, and the Royal College of Physicians of London, the following qualifications are provided by MRCP (UK):
- MRCP (UK) Diploma
- 12 Specialty Certificate Examinations (SCEs)
What are Specialty Certificate Examinations (SCEs)?
These examinations are a chance to evaluate the candidate’s knowledge of the globally set standard. SCEs cover all that’s required to know, by a newly qualified specialist in the chosen field. These are required for specialist physicians in the UK.
What is the Difference Between MRCP Part 1 and Part 2?
Understand it as ‘MRCP Part 1 being the foundation where basic medical and clinical knowledge is tested’ and ‘MRCP Part 2′ being the practical application of what the medical professional has learnt!’
| MRCP Part 1 | MRCP Part 2 |
| Foundation of Basic Medical Knowledge | Practical Application of What’s Leant |
| MCQ Style Questions | Image Based Questions & Clinical/Medical Scenarios |
| Tests Common Disorders & Clinical Sciences | Evaluates Decision Making/Reactions Under Pressure |
What are MRCP Part 1 Dates 2024?
Mark your calendars! Here are the crucial upcoming dates for the MRCP Part 1 exam in 2024:
- 14 August 2024: Application period from 3 June to 10 June 2024.
- Results by 13 September 2024.
- 16 October 2024: Application period from 5 August to 12 August 2024.
- Results by 15 November 2024.
- 22 January 2025: Application period from 4 November to 11 November 2024.
- Results by 21 February 2025.
- 16 April 2025: Application period from 3 February to 10 February 2025.
- Results by 16 May 2025.
This calendar is a reminder of stepping closer to your goal. So, plan and prepare for MRCP beforehand to be all set when the time comes.
What is MRCP PART 1 Exam Syllabus and Format?
The MRCP Part 1 exam is composed of two papers, each with 100 MCQs. Total time is three hours to complete the exam. Here’s a snapshot of what you need to cover for the exam. Don’t forget to revise all of it.
How to prepare MRCP PART 1? (Key Concepts)
Here’s the snapshot of what needs to be grasped!!!
- Cardiology: Heart diseases, ECG interpretation
- Respiratory Medicine: Asthma, COPD
- Gastroenterology: Liver diseases, inflammatory bowel disease
- Neurology: Stroke, epilepsy
- Endocrinology: Diabetes, thyroid disorders
- Rheumatology: Arthritis, connective tissue diseases
- Nephrology: Acute kidney injury, chronic kidney disease
- Infectious Diseases: HIV, tropical diseases
- Hematology: Anemias, clotting disorders
- Oncology: Cancer types, treatments
- Psychiatry: Mood disorders, schizophrenia
- Ophthalmology: Eye diseases, vision tests
- Dermatology: Skin infections, dermatologic conditions
- Clinical Pharmacology: Drug mechanisms, side effects
How to Prepare MRCP Part 1? (Tips & Tricks)
Preparation is the key to success! For cracking MRCP Part 1, a smart/strategic vision can make all the difference. Here are some tips to get you started:
- Always Make a Plan: Note down topics and make a well-structured study plan.
- Use Quality Resources: Enroll for digital courses and classes, and start a guided journey. One such being ‘Cracking MRCP Part 1’ by Dr Gurpreet Singh Wander and Dr Archith Boloor.
- Practice Makes a Man Perfect: Practice the MCQs, solve question banks, and research online. A good digital course will always provide you practice exercises too.
- Join Study Groups: A collective learning can assist you get different perspectives and clarify doubts. Join online forums or local study groups to discuss tricky topics.
- Keep a Note of UK Medicine Area: Indian students need to have an edge over this! A candidate must have knowledge of UK internal medicine training, UK’s guidelines, and other important breakthroughs in UK medical science.
It is a difficult exam but only for those who do not prepare! Just be on time. From online application dates to having a note of closing deadline, from initial preparation of sample questions to final exam preparation, leave no chance for delays. Also, stay stress-free, especially on the exam day to have 100% chance of success. Stress is the biggest enemy. So, to win over a wide range of subjects from the syllabus, just be confident and stress-free.
What is the MRCP Part 1 Fees in India?
While enrolling, the Indian students registering from India need to pay around £616 as fee for the MRCP Part 1 exam as they are international students. For the UK, the application procedures include fee as £460. The fees may vary, so it’s best to check the MRCP UK website for the latest information.
To be eligible for the MRCP Part 1 exam, a candidate must:
- Hold a medical degree recognized by the General Medical Council (GMC) or equivalent.
- Have completed at least one year of postgraduate medical experience.
Understanding MRCP Part 1 Results
The MRCP Part 1 results are usually released 4 to 6 weeks after the exam. The results are published online on the MRCP UK website, where you can log in to view your scores. The pass mark usually hovers around 540, but it’s adjusted based on the exam’s difficulty through a process called equating.
Final Thoughts
The MRCP Part 1 exam is a crucial milestone in a medical career. With a detailed understanding of the schedule, key dates and prep strategies, this exam can be cracked! With the right resources, regular practice, and staying up to date with official updates and news, a candidate can pass this exam with flying colors. Let’s remember, the MRCP Part 1 is not just an exam; it’s a steppingstone to a fulfilling career in medicine. Your journey to becoming a specialist physician begins here!
Note: For more detailed information and to stay updated with the latest announcements, visit the MRCP UK website.
Frequently Asked Questions (FAQs)
Q1. What is the MRCP Exam 1 Format?
Ans. Exam Format is as follows:
- The MRCP Part 1 exam consists of two 3-hour papers.
- It is in the MCQ (Multiple-Choice-Questions) format.
Q2. What is the MRCP Part 2 Exam Format?
Ans. The MRCP Part 2 is further in two parts. One is Written and the other is Clinical Examination, known as PACES.
- The ‘Written’ consists of a three-hour MCQ based question paper including diagnosis, investigations & prognosis of patients.
- The ‘PACES’ includes 5 clinical stations series, each evaluated by two examiners.
Q3. When can we Register for the Upcoming MRCP Part 1 Exam?
Ans. At present, application process can start from 5th August to 12th August 2024. It is for the exam to be held on 16th October, 2024. The results could be out by 15th November, 2024. The rest of examination dates have been mentioned above in the blog, in detail.
Q4. What is the fee for MRCP Part 1 Exam?
Ans. The fee is around £460 for (UK) and £616 for international students. However, there could be slight changes in the fee depending upon various factors. It is always advisable to reach out to the official website of MRCP for the exact fee structure.
Everything is made for a defined purpose anything which is not intended for further use is termed waste. In the scientific and industrial eras combined with the increasing population, the turnover of products has gone very high increasing the quantum of urban solid waste. With the increased need for health care in a changing society the role of hospitals/nursing homes comes to the forefront.
Hospital waste or types of healthcare waste should include any material generated in healthcare establishments including aqueous and other liquid waste.
Hospital waste means any solid, fluid, or liquid waste material including its container and any other intermediate product which is generated during short-term and long-term care consisting of observational, diagnostic, therapeutic, and rehabilitative services for a person suffering or suspected to be suffering from disease or injury and for parturient or during research of production and testing of biological during immunization of human being.
Types of Healthcare waste facilities are responsible for managing healthcare waste generated within their facilities, as well as waste generated through activities in the community. These facilities must undertake proper segregation, collection, in-house transportation, pre-treatment, and waste storage before handing it over to a Common Bio-medical Waste Treatment Facility (CBWTF) operator.
Therefore, proper management of healthcare waste at these facilities necessitates that all categories of staff understand and adhere to the technical requirements for waste handling as per the Biomedical Waste Management Rules, 2016.
Classifications of Waste Generated from Healthcare Sectors
1. Bio-Medical Waste
It refers to any waste produced during diagnosis, treatment, or immunization of humans or animals as well as related research activities, or during the production or testing of biologicals in health camps. This includes all waste from healthcare facilities that could potentially harm human health or the environment if improperly disposed of. Such waste is considered infectious and must be managed according to the Biomedical Waste Management Rules of 2016 to prevent adverse effects on health or the environment.
Around 10% to 15% of the total waste generated by healthcare facilities constitutes biomedical waste. This category includes materials that have come into contact with patients’ blood, secretions, infected body parts, biological fluids, chemicals, medical equipment, pharmaceutical waste, laboratory discharge, sharp objects like needles and glassware, and plastics.
According to the Biomedical Waste Management Rules of 2016, this waste is categorized into four types based on how it is segregated and color-coded. Each category includes specific types of biomedical waste, as given below:
- Yellow Category
- Red Category
- White Category
- Blue Category
These categories are divided as per the types of waste under each category as follows:
| Category | Type of Waste |
| Yellow | Human Anatomical Waste
Human tissues, organs, body parts, and fetus below the viability period (as per the Medical Termination of Pregnancy Act 1971, amended from time to time). |
| Animal Anatomical Waste
Experimental animal carcasses, body parts, organs, and tissues, including the waste generated from animals used in experiments or testing in veterinary hospitals or colleges, or animal houses. |
|
| Solid Waste
Items contaminated with blood, body fluids like dressings, plaster casts, cotton swabs, and bags containing residual or discarded blood and blood components. |
|
| Discarded Medicine
Pharmaceutical waste like antibiotics, and cytotoxic drugs including all items contaminated with cytotoxic drugs along with glass or plastic ampoules, and vials. Etc. |
|
| Chemical Waste
Chemicals used in the production of biological and used or discarded disinfectants. |
|
| Chemical Liquid Waste
Liquid waste is generated due to the use of chemicals in the production of biological and used or discarded disinfectants, Silver X-ray film developing liquid, discarded Formalin, infected secretions, aspired body fluids, liquid from laboratories, and floor washings, cleaning, housekeeping and disinfecting activities, etc. |
|
| Discarded linen, mattresses, beddings contaminated with blood or body fluid, routine mask & gown. | |
| Microbiology, Biotechnology, and other clinical laboratory waste (Pre-treated) | |
| Microbiology, Biotechnology, and other clinical laboratory waste: Blood bags, laboratory cultures, stocks or specimens of microorganisms, live or attenuated vaccines, human and animal cell cultures used in research, industrial laboratories, production of biological, residual toxins, dishes, and devices used for cultures. | |
| Red | Wastes are generated from disposable items such as tubing, bottles, intravenous tubes and sets, catheters, urine bags, syringes without needles, fixed needle syringes with their needles cut, vacutainers, and gloves. |
| White | Waste Sharps Including Metals
Needles, syringes with fixed needles, needles from needle tip cutters or burners, scalpels, blades, or any other contaminated sharp object that may cause punctures and cuts. This includes both used, discarded, and contaminated metal sharps. |
| Blue | Broken or discarded and contaminated glass including medicine vials and ampoules except those contaminated with cytotoxic wastes. |
2. General Waste
General waste includes all waste other than biomedical waste that has not been in contact with hazardous waste or infectious materials, chemicals, or biological secretions, and does not include sharp objects. This type of waste typically includes:
- Newspaper, paper, and cardboard boxes
- Plastic water bottles
- Aluminum cans from soft drinks
- Packaging materials
- Food containers after removing leftover food
- Organic or biodegradable waste, mainly food waste
- Construction and demolition waste
These general wastes are classified as wet wastes and dry wastes and should be collected separately. The quantity of general waste is around 85% to 90% of the total generated from the facility.
3. Other Wastes
Other wastes include electronic devices such as batteries and radioactive materials that are not classified as biomedical waste. They must be disposed of according to specific regulations: the E-waste (Management) Rules of 2016, the Batteries ( Management & Handling) Rules of 2001, and the rules or guidelines established under the Atomic Energy Act of 1962, depending on the type of waste generated.
Guidelines for Management of Healthcare Waste Categories as per Biomedical Waste Management Rules, 2016
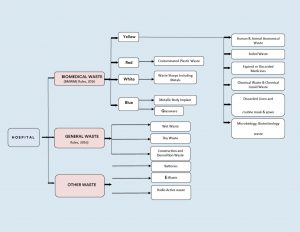
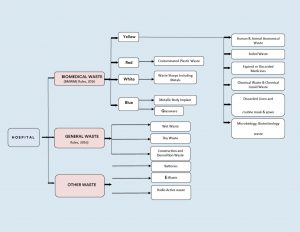
Figure 1: Categorization & Classifications of Wastes in Health Care Facilities.
Color Coding and 4 types of dustbins in hospitals used for Waste Segregation & Collection
According to Schedule I of the Bio-Medical Waste Management Rules of 2016, healthcare facilities (HCFs) must use specific color-coded dustbins and types of containers/bags for segregating and collecting biomedical waste generated within the facility.
| Category | Type of Waste | Colored Container & Type of Container | Treatment Options as per Schedule I |
| Yellow Category |
|
Yellow-colored non-chlorinated Plastic Bags.
NOTE: |
Incineration/deep burial |
| Red Category |
|
Red Colored Non-Chlorinated Plastic Bags (having thickness equal to more than 50u) and containers. | Autoclaving/microwaving/chemical treatment |
| White Category |
|
White Colored translucent puncture-proof, leak-proof, tamper-proof containers. | Autoclaving/microwaving/chemical treatment and destruction/shredding |
| Blue Category |
|
Puncture-proof, leak-proof boxes or containers with blue-colored markings. | Disposal of wastes and secured landfill |
Bio-Medical Waste Collection
Time of Collection
- Daily Collection: Ensure daily collection from each hospital ward at fixed intervals.
- Timing Adjustments: Schedule collections based on waste generation patterns throughout the day.
- Separate Collection: Avoid collecting general waste concurrently with biomedical waste.
- Visitor Waste Management: Collect general waste immediately after visiting hours to prevent accumulation.
- Personal Protective Equipment: Provide PPE to staff handling biomedical waste.
Packaging
- Filling and Sealing: Fill biomedical waste bags and sharp containers up to three-quarters full and seal them promptly.
- Sealing Methods: Use ties or plastic tags to seal bags to avoid stapling.
- Availability of Replacement: Ensure replacement bags or containers are readily available at collection points.
- Labeling Requirements: Label bags and containers with biohazard symbols, including details like date, type of waste, quantity, and sender’s and receiver’s information.
- Barcode Compliance: Affix barcoded labels on the bag as per CPCB guidelines.
Labeling
- Biohazard Symbols: Clearly label all bags, containers, and bins with biohazard or cytotoxic symbols as per BMWM Rules, 2016.




Interim Storage
- Minimization: Discourage interim storage of biomedical waste in patient care areas.
- Designated Areas: Store biomedical waste temporarily in designated, low-traffic areas if necessary.
Treatment Option for Bio-medical Waste Types
| Treatment Options | Biomedical Chemical Processes |
| Thermal Processes Low-heat Systems (93-177oC) |
|
| High-heat Systems |
|
| Mechanical Processes |
|
| Irradiation Processes |
|
| Biological Processes |
|
| Considerations for Processing Incineration |
|
| Autoclaving |
|
| Microwaving |
|
| Deep Burial |
|
| Sharp Materials Disposal |
|
| Radioactive Waste |
|
| Mercury Control |
|
Frequently Asked Questions (FAQs)
Q1. What is clinical waste, and how is it different from infectious waste?
Ans. Clinical waste includes all waste generated from medical facilities, including non-infectious materials like packaging and expired medications, whereas infectious waste refers to waste contaminated with pathogens, such as bacteria, viruses, or other microorganisms.
Q2. What are the proper disposal techniques for biomedical waste, particularly sharps waste?
Ans. Sharp waste like needles and scalpels, must be disposed of in puncture-proof containers specifically designed for sharps disposal. These types of containers are sealed and handled carefully to prevent injuries and potential infections during disposal.
Q3. How does improper medical waste management contribute to the spread of diseases?
Ans. Improper management of biohazardous waste can lead to contamination of the environment and increase the risk of spreading infectious diseases. Pathogens present in medical waste, if not managed correctly, can infect healthcare workers, patients, and the normal public.
Q4. What is some risk associated with inadequate handling of pathological waste?
Ans. Pathological waste which includes tissues, organs, and body parts, poses significant health risks if not properly managed. Exposure to such waste can lead to infections or exposure to hazardous chemicals used in treatments.
Q5. Why is it important for medical facilities to use appropriate medical waste containers?
Ans. Medical waste containers are designed to safely store and transport various types of medical waste, including biohazardous materials and sharps. Using proper containers minimizes the risk of accidental exposure and ensures compliance with regulations for safe disposal.
DigiNerve is constantly evolving to enhance your experience while you’re on your journey to becoming a Top Doc. We are excited to bring you the latest updates with our commitment to ensure a seamless journey on the go.
Read on the July edition (Vol – 1) of our monthly newsletter to know the latest updates.
CONTENT UPDATES
PostGrad Course Updates
Dermatology MD:-
1. Chat show on ‘Discussion on Leprosy’ by Dr. Vivek Vasudev Pai, Dr. Shraddha Mahobia, and Dr. Samira Siddiqui Khatoon Mohd. Hanif has been added to the course.
Learning Outcomes of the chat show were:
- To learn the approach to a patient with leprosy.
- To understand the current scenario of leprosy and the National Strategic Plan for 2023-2027 for India.
- To learn the approach to patients with lepra reactions and relapse.
- To understand the management of patients with ENL reactions and relapse.
Pediatrics MD:-
1. Chat show on ‘Approach to a Child with Asthma’ by Dr. Piyush Gupta and Dr. Prawin Kumar has been added to the course.
Learning Outcomes of the chat show were:
- Clinical presentation of asthma in children.
- How can a diagnosis of asthma in children be established?
- What is the role of the Pulmonary Function Test (PFT) in the diagnosis of asthma.
- Management of Asthma in Children.
Medicine MD:-
1. 8 new topics have been added to the following modules:
| Module | Section | Topic |
| Rheumatology | Long Case Discussions | Gout |
| Infectious Diseases | Clinical Scenarios | Amoebic Liver Abscess |
| Systemic Fungal Infections | ||
| Japanese Encephalitis | ||
| Critical Care Medicine | Decision Making | Central Venous Line |
| Intubation in Critically Ill Patients | ||
| Cardiology | Basic Sciences | Treadmill Test |
| Endocrinology and Diabetes | Long Case Discussions | Approach and Management of Hyponatremia |
Note: The topics mentioned above also include 39 new self-assessment and 16 benchmark trials.
Update Your DigiNerve App for Better Experience.
To read the updates shared in the Monthly Newsletter June (Vol-2), click here.
DigiNerve is constantly evolving to enhance the user experience while you’re on their journey to becoming a Top Doc. We are excited to bring the latest updates with our commitment to ensure a seamless journey on the go.
Read our monthly newsletter’s June edition (Vol – 2) for the latest updates.
CONTENT UPDATES
PostGrad Course Updates
OBGYN MD:-
1. 5 new topics have been added to the following modules:
| Section | Module | Topic |
| Gynecology | Menstrual Abnormalities | Menopause Hormonal Therapy |
| Obstetrics | Procedural Videos | Caesarean Section |
| Third Stage of Labour and its Complications | Postpartum Psychiatric Illness | |
| Medical Disorders in Pregnancy | Case Discussion: Pregnancy Induced Hypertension | |
| Labour (Normal and Abnormal) | Management of Abnormal Labour |
Note: The topics mentioned above also include 25 new MCQs and 10 benchmark trials.
2. Chat show on ‘Primary Amenorrhea’ by Dr. Aswath Kumar and Dr. Lilly Varghese has been added to the course:
Learning Outcomes of the chat show were:
- Different etiologies of primary amenorrhea
- Important subtypes: Clinical features
- Investigations
- Management: Hormonal and surgical treatment
Surgery MS:-
1. Chat show on ‘Management of Head Injury’ by Prof. (Dr.) Nilay Mandal and Dr. Arjun Dasgupta has been added to the course.
Learning Outcomes of the chat show were:
- Initial assessment of a head injury patient
- Prevention of secondary injury and management of raised ICP
- Types of head injury and their radiological findings
Professional Course Updates
MRCOG Part 2:-
1. Webinar on ‘Discussion of Important Questions and Doubt Clearance (MRCOG-2 EMQs)’ by Dr. Richa Saxena has been added to the course.
Learning Outcomes of the webinar were:
- To discuss important questions of MRCOG part 2 exam.
- To prepare for exam with the help of carefully curated questions with detailed explanations, images and flowcharts.
- To ease the journey of clearing MRCOG exam.
- To understand latest patterns of questions as per RCOG curriculum (EMQs).
Technology Updates
1. Inclusion of HYQs
A new section of High Yield Questions has been included in the courses- Cracking MRCOG- PART 1 and Part 2. It comprises HYQs from the year 2016-2022.
2. Free Access to Dr. Wise
An additional benefit of 10 queries for non-subscribers.
3. Customised Question Bank Generator
- A new feature of Customised Question Bank Generator has been added, under the course of Cracking MRCOG Part-1.
- Beneath the ‘Test’ section, users can generate questions in the ‘Practice’ or ‘Test Mode’ as per the choice of difficulty level and as per the number of questions required.
Update Your DigiNerve App for Better Experience.
To read the updates shared in the Monthly Newsletter July (Vol-1), click here.
Clearing MBBS is itself a difficult task and then cracking competitive exams is another level of challenge. But you can’t skip this challenging situation if you want to the accelerating graph of your career.
Success in the MRCP Part 1 exam signifies that you have not only retained the knowledge you learned during your undergraduate studies but that it has also grown to keep up with developments that have happened since you graduated and continues to serve as a foundation for clinical decision-making.
Most important to note, MRCP is just a pass or fail exam.
Step-by-Step Study Guide for MRCP Part 1 Exam
1. Understand the Exam Pattern.
MRCP Part 1 is a single-day Computer-based exam comprising two papers. Each paper has 100 multiple-choice questions to be solved in three hours. The MCQs follow the ‘best of five’ exam format. No negative marking gives a bit of relaxation for this competitive exam.
This MRCP Part 1 overview will let you get familiar with the exam pattern and will help you plan your preparation and revision strategy with effective time management. It is crucial to distribute the time to learn each specialty depending on the vastness of the subject, subject weightage, your level of understanding of the subject, etc.
Click here to learn the subject- weightage/blueprint of the MRCP Part 1 exam.
2. Choose your Exam Date Wisely.
It is advised to give the MRCP Part 1 first attempt after 12-24 months of graduation. Once you feel confident enough to take an exam, then only register for it. Usually, competitive exams are held once or twice a year, but the MRCP Part 1 exam occurs four times a year (January/April/August/October), which provides an opportunity for you to apply as per your suitability. You don’t have to wait for another year to sit the exam if you don’t want to sit for the exam this time.
3. Start Preparing Early.
Given how difficult the MRCP Part 1 test is, it’s crucial to give yourself plenty of time to study. Give a minimum of 6-10 months for sincere preparation. Don’t get confused; talk to seniors, faculty, friends, or mentors to get the best advice for you. Early preparation saves your time and boosts your confidence. Effective planning and consistency pave the way to effective results.
4. Make a Realistic Study Plan.
Create an MRCP Part 1 study plan that describes the material you will cover each day or week after you have your study materials. Allocate the time to a particular specialty keeping the factor in mind that your level of understanding is at beginner level or intermediate. Also, consider that there is enough time left for revision and practice questions. Revision strategy is also a must so that you don’t miss out on anything at the eleventh hour. Practice the question according to the exam pattern to get more familiar with it and this will also enhance your ability to tackle a question in the exam. Review your performance and revise your strategy accordingly.
5. Stick to Reliable Study Resources.
There are several options for MRCP Part 1 study materials, including books, online MRCP 1 exam resources, and question banks. To have a thorough grasp of the subject, it’s crucial to employ a range of materials, and resource selection is recommended. The preferred books for MRCP Part 1 are “Mastering Medicine: MRCP Made Easy” by Dr. Archith Boloor, Essential Revision Notes for MRCP by Philip A. Kalra, and the Oxford Handbook of Clinical Medicine by R.A. Hope. For online MRCP preparation may it be video lectures or Practice questions, you can subscribe to the ‘Cracking MRCP Part 1’ course. You can attend webinars and exam discussion videos only by the eminent faculty.
6. Enroll in online MRCP part 1 preparation courses.
To ace your MRCP preparation, you can enroll in one of the best online courses for MRCP Part 1, “Cracking MRCP Part 1” by eminent faculty, Dr. Gurpreet Singh Wander and Dr. Archith Boloor. The course covers modules covering all the major specialities and is devised based on The Royal College of Physicians curriculum. Every module in the Cracking MRCP Part 1 study materials includes webinars and video archives, approx. 2000 best of five MCQs/MRCP Part 1 practice questions, notes, high-yielding questions, e-chapters, and performance tracking. It additionally benefits you with the mock papers intended to give a feel of a real exam. The leaderboard ranking feature of the course enables you to track your performance and prepare accordingly. To ease the preparation and revision, the Cracking MRCP Part 1 notes are categorised into three sections: Wake-up calls, Golden signs, and Clinical gems. The Wake-up calls indicate the red flag signs pointing towards a certain disease or condition, Golden signs signify characteristic diagnostic features of a disease or condition, and Clinical gems signify recommended management or preferred drug choice for a disease or condition.
7. Don’t Miss Out on High-Weightage Topics.
A wide number of subjects are covered in the MRCP Part 1 exam; however, some are assessed more rigorously than others. The following are the high-weightage speciality/subjects:
- Cardiology
- Clinical Pharmacology and Therapeutics
- Clinical Sciences
- Endocrinology, Diabetes, and Metabolic Medicine
- Gastroenterology and Hepatology
- Infectious Diseases
- Neurology
- Renal Medicine
- Respiratory Medicine
- Rheumatology
8. Practice Mock Exams and Previous Year Papers.
Practicing mock exams and previous year’s papers is an excellent method to gauge your progress and determine where you need to concentrate and revise your strategy. There are a variety of mock tests accessible, both online and in books. DigiNerve with the Cracking MRCP Part 1 online course gives access to the free mock paper. You must attempt it under the timed condition for self-evaluation. Utilising question banks for practise will give you a better understanding of the questions that are asked.
9. Be Consistent and Manage Time Effectively.
Consistency is the key. Although taking the MRCP Part 1 test might be nerve-wracking, it’s crucial to remain composed and concentrated. Be consistent with your study routines along with balancing clinical practice.
Also, time management skills are crucial because the MRCP Part 1 test is timed. Give yourself enough time to respond to each question but avoid spending too much time on a single question. Mark the question for review if you are unsure about the answer, then go on. If you have time, you can return to the marked questions later. Remind yourself that you are prepared for the exam by taking deep breaths.
10. Take Good Care of your Health.
Consume healthful meals and get adequate sleep. Good health improves concentration and memory. Don’t get stressed a lot and meditate regularly because mental health is as important as physical health. Especially on the day of the exam, it’s critical to obtain adequate sleep and consume a balanced diet. You’ll be able to focus and remain awake as a result.
MRCP Part 1 Exam Day Tips
- Get familiar with the route and location of the exam centre and reach on time on exam day.
- Don’t be late for Paper-II after the break. It is advised to be at your desk at least 15 minutes before Paper-II is about the start.
- You are not allowed to take any items, accessories, or stationary along with you in the exam.
- The required stationery items are provided in the exam hall itself.
- Don’t wear hoods for the exam.
- Keep your ID handy for entry and checking purposes.
Frequently Asked Questions (FAQs)
Q1. What score do you need to pass MRCP Part 1?
Ans. The pass marks for MRCP Part 1 are around 540. The Equating process based on Response theory is used to calculate the candidate’s overall result. The pass marks are calculated as the overall scaled score unlike other exams, where the overall percentage score is considered.
Q2. Is there a negative marking in MRCP Part 1?
Ans. No, there is no negative marking in the MRCP Part 1. This is a great advantage for all the candidates aiming to clear the MRCP exam.
Q3. Is MRCP difficult to pass?
Ans. Undoubtedly, the MRCP exam is difficult to pass but not impossible. With smart study, consistent efforts, proper clinical practice, and effective time management, you can crack the MRCP exam.
The UPSC CMS is an abbreviation for “Union Public Service Commission-Combined Medical Services” Examination. It is a competitive examination that the Union Public Service Commission (UPSC) of India administers. The CMSE is held every year to fill various medical positions in government agencies including the Indian Railways, Central Health Service, Municipal Corporation of Delhi, and several other central government health institutions. The CMS exam allows medical professionals to join the esteemed Indian government healthcare service organizations and support the country’s healthcare system.
The difficulty level of the exam is self-explanatory by the term UPSC; UPSC CMSE is a hard nut to crack. With smart study, consistent efforts, and a lot of practice, you will pass with flying colours. Make sure to start early and stick to a realistic study plan and reliable study resources.
In this blog, you will get detailed information about the UPSC CMS exam recruitment category, eligibility criteria, exam pattern, selection procedure, and syllabus.
To be eligible to sit in the exam, a candidate must be either:
(a) an Indian citizen, or
(b) a subject of Nepal, or
(c) a subject of Bhutan, or
(d) a Tibetan refugee who came over to India before the 1st January 1962 to permanently settle in India, or
(e) a person of Indian origin who has migrated from Pakistan, Burma, Sri Lanka, or East African Countries of Kenya, Uganda, the United Republic of Tanzania, Zambia, 6 Malawi, Zaire, and Ethiopia or Vietnam to permanently settle in India.
Provided that a certificate of eligibility has been issued by the Government of India in favour of the candidate belonging to categories (b), (c), (d), and (e) mentioned above.
UPSC CMS Recruitment Category
UPSC CMS exam is conducted for the recruitment for the following categories and positions:
Category-I:
Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services
Category-II:
Assistant Divisional Medical Officer in the Railways
General Duty Medical Officer in New Delhi Municipal Council
General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
There are reservations for candidates belonging to Scheduled Castes, Scheduled Tribes, Other Backward Classes, Economically Weaker Sections, and Persons with Benchmark Disability as per the vacancies by the Government.
UPSC CMS Exam Pattern
Medical graduates with an MBBS degree along with completion of internship are eligible to apply for the UPSC CMS exam. There are two parts of CMSE, one is a written examination and the other is an interview. The CMSE comprises two theory papers followed by a personality test or interview. Here’s a breakdown of the exam pattern:
Part-I: Written Examination
The written examination comprises two papers:
Paper-I: This paper includes questions from General Medicine and Pediatrics subject. The exam Pattern 2024 for UPSC CMSE Paper-I is mentioned in the below table:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper I | 120 (96 questions from General Medicine and 24 from Pediatrics) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Paper-II: This paper includes questions from Surgery, Obstetrics & Gynecology, and Preventive and Social Medicine subjects. The Surgery subject also includes ENT, Ophthalmology, Traumatology, and Orthopaedics subjects. The table below mentions the exam scheme for UPSC CMSE Paper-II 2024:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper II | 120 (40 questions from each subject, Surgery, OBGYN, and Community Medicine) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Part-II: Interview/Personality Test
After passing the written test, candidates are invited by the Union Public Service Commission for an interview/personality test to determine their fit for the open positions.
The personality test carries 100 marks. The interview is designed to complement the written examination for measuring the general knowledge and academic study skills of the applicants as well as to function as a personality test to evaluate the candidate’s critical thinking skills, absorption capacity, and overall capacity for social cohesiveness, sound judgment, and moral character, initiative, and leadership potential. Basically, it aims to assess the candidate’s personality, communication skills, and suitability for the posts in medical services.
Final Selection
The final selection is done based on the combined marks obtained in Paper-I, Paper-II, and the Interview/Personality test.
Recruitment of a number of candidates is based on the vacancies in the particular position. Succeeding applicants are assigned to different Group-A positions within the public health system. The particular positions and openings change every year.
It’s significant to note that the Paper-I and Paper-II syllabuses contain a broad variety of medical science-related topics. A wide range of medical topics, including clinical disciplines, general knowledge, and current events, are covered in the CMSE curriculum. To score well on the test, candidates must have a solid comprehension of these topics. It is a crucial aspect of a good preparation strategy to know and understand the syllabus of the CMS exam. It leads to effective time management.
UPSC CMS Syllabus
UPSC CMS Syllabus Paper I:
General Medicine subject includes the following topics:
- Cardiology
- Respiratory diseases
- Gastro-intestinal
- Genito-Urinary
- Neurology
- Hematology
- Endocrinology
- Metabolic disorders
- Infections/Communicable Diseases
-
- Virus
- Rickets
- Bacterial
- Spirochetal
- Protozoan
- Metazoan
- Fungus
- Nutrition/Growth
- Diseases of the skin (Dermatology)
- Musculoskeletal System
- Psychiatry
- General
- Emergency Medicine
- Common Poisoning
- Snakebite
- Tropical Medicine
- Critical Care Medicine
- Emphasis on medical procedures
- Patho physiological basis of diseases
- Vaccines-preventable diseases and Non-vaccines preventable diseases
- Vitamin deficiency diseases
- In psychiatry – Depression, psychosis, anxiety, bipolar diseases, and Schizophrenia
Pediatrics subject includes the following topics:
- Common childhood emergencies
- Basic newborn care
- Normal developmental milestones
- Accidents and poisonings in children
- Birth defects and counselling including autism
- Immunization in children
- Recognizing and managing children with special needs
- National programmes related to child health
UPSC CMS Syllabus Paper II:
Surgery subject includes the following topics:
- General Surgery
- Wounds
- Infections
- Tumours
- Lymphatic
- Blood vessels
- Cysts/sinuses
- Head and neck
- Breast
- Alimentary tract
-
- Oesophagus
- Stomach
- Intestines
- Anus
- Developmental
-
- Liver, Bile, Pancreas
- Spleen
- Peritoneum
- Abdominal wall
- Abdominal injuries
- Urological Surgery
- Neurosurgery
- Otorhinolaryngology/E.N.T.
- Thoracic surgery
- Orthopaedic surgery
- Ophthalmology
- Anaesthesiology
- Traumatology
- Diagnosis and management of common surgical ailments
- Pre-operative and post-operative care of surgical patients
- Medico-legal and ethical issues of surgery
- Wound healing
- Fluid and electrolyte management in surgery
- Shock pathophysiology and management
Obstetrics and Gynecology subject includes the following topics:
- Questions on applied anatomy
- Questions on applied physiology of menstruation and fertilization
- Questions on infections in the genital tract
- Questions on neoplasm in the genital tract
- Questions on displacement of the uterus
- Normal delivery and safe delivery practices
- High-risk pregnancy and management
- Abortions
- Intra Uterine growth retardation
- Medicolegal examination in OBGYN including the rape
Family Planning subject includes the following topics:
- Conventional contraceptives
- D. and oral pills
- Operative procedure, sterilization, and organization of programmes in the urban and rural surroundings
- Medical Termination of Pregnancy
Preventive Social & Community Medicine subject include the following topics:
- Social and Community Medicine
- Concept of Health, Disease and Preventive Medicine
- Health Administration and Planning
- General Epidemiology
- Demography and Health Statistics
- Communicable Diseases
- Environmental Health
- Nutrition and Health
- Non-communicable Diseases
- Occupational Health
- Genetics and Health
- International Health
- Medical Sociology and Health Education
- Maternal and Child Health
- National Programmes
- Management of common health problems
- Ability to monitor national health programmes
- Knowledge of maternal and child wellness
- Ability to recognize, investigate, report, plan, and manage community health problems including malnutrition and emergencies.
You can also enroll in online MBBS courses to get conceptual clarity over MBBS subjects by the top medical faculty of India. You have the opportunity to learn and get your concepts clear in Surgery by Dr. Sriram Bhat M, Microbiology by Dr. Apurba S Sastry, Dr. Sandhya Bhat and Dr. Deepashree R, Medicine by Dr. Archith Boloor, Pathology by Prof Harsh Mohan, Prof Ramadas Nayak, and Dr. Debasis Gochhait, and similarly other MBBS subjects by subject’s eminent faculty. The comprehensive knowledge of MBBS subjects and problem-solving capabilities will directly impact your CMS exam.
Frequently Asked Questions (FAQs):
Q1. Is UPSC CMS conducted every year?
Ans. Yes, the UPSC CMS exam is conducted every year and the recruitment is based on the number of vacancies for a particular post in various government health organizations.
Q2. What is a career after CMS?
Ans. UPSC CMSE is conducted for the recruitment of the Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services, Assistant Divisional Medical Officer in the Railways, General Duty Medical Officer in New Delhi Municipal Council, and General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
Q3. Who conducts the CMS exam?
Ans. The CMS exam is a competitive examination conducted by the Union Public Service Commission (UPSC) of India.
Q4. What is the pattern of UPSC CMS exam?
Ans. There are two parts of CMSE in which part-I is a written examination and the part-II is an interview. The CMSE comprises two theory papers followed by a personality test or interview.
The Part-I written examination comprises two papers: Paper-I and Paper-II.
The National Medical Commission (NMC) has achieved the coveted World Federation for Medical Education (WFME) Recognition Status for a tenure of 10 years. This is a prestigious achievement for India’s medical education. This esteemed award proves NMC’s steadfast dedication to the highest standards in medical education and accreditation.
The WFME recognition will now enable Indian medical graduates to pursue postgraduate training and practice in other countries that require WFME recognition, such as Australia, USA, Canada, and New Zealand.
The World Federation for Medical Education (WFME) is a global organization dedicated to raising the standard of medical education all over the world. The WFME accreditation programme is crucial in ensuring that medical institutions uphold and adhere to the highest levels of global education and training standards.
Dr. Yogender Malik, Member of the Ethics and Medical Registration Board and Head Media Division at NMC, on this remarkable achievement, said, “WFME’s recognition underscores that the quality of medical education in India adheres to global standards. This accolade empowers our students with the opportunity to pursue their careers anywhere in the world, while also making India an attractive destination for international students due to our globally recognized standards.”
Under this accreditation, all the 706 existing medical colleges in India will be considered WFME accredited, and the new colleges being set up in the coming 10 years will also be considered as WFME accredited. This will also benefit NMC in enhancing the quality and standards of Indian medical education by aligning them with global benchmarks. This will facilitate academic collaborations and promote continuous improvement and innovation in medical education.
Now NMC being WFME accredited has opened the doors for all the medical students for ECFMG and USMLE. All Indian students will become eligible to apply for the Education Commission on Foreign Medical Graduates and United States Medical Licensing Examination.
The National Medical Council, Ministry of Health and Family Welfare in a press release dated 20th September 2023 has announced this remarkable update.
Global health comprises the biological and clinical facets of diseases along with the social, economic, political, and environmental determinants of health. The ability to confine health issues inside national borders has diminished as the globe becomes more linked.
The contribution of technology to the medical sector is unparalleled. With the years passing by technology is improving at the highest pace in the medicine sector. Nowadays, the use of AI, and the development of new therapies, drugs, drug development, and surgical procedures, have made complex medical procedures less complex and paved a path to minimally invasive surgeries. Millions of individuals throughout the world are having their lives improved as a result of these developments.
Global health has improved recently despite several obstacles like poverty, pandemics, disease outbreaks, conflicts, and climate change. Maternal and child fatalities have dropped significantly and since the development of new vaccinations, infectious illness spread has also been reduced. Governments and organisations have also boosted their funding for global health concerns and also significantly invested in newer technologies. The current developments in the healthcare industry are beneficial to global health and are an area with significant potential to enhance the health of people all over the world and in the medical field. We can improve the health of people all across the world by addressing the issues and embracing the possibilities.
Medical students and professionals must keep themselves updated and knowledgeable about the recent advancements in healthcare as it is going to impact their career growth to a great extent. To escalate the growth of your medical career, it is mandated to upskill.
The recent advancements in the global healthcare and medicine field are significant for several reasons. By offering more precise diagnoses, earlier illness detection, and more individualised treatment regimens, they have the potential to:
- Improve the quality of care for patients.
- By enabling remote monitoring and care and minimising the need for in-person visits, healthcare may be made more accessible and cheaper.
- Increase the effectiveness of healthcare delivery by simplifying administrative procedures and facilitating information exchange between healthcare professionals.
- Develop novel therapies and preventative measures to lessen the impact of chronic illnesses.
- Boost public health by keeping track of and rapidly and efficiently addressing illness outbreaks.
Below mentioned are technological advancements in medicine and global healthcare:
Artificial Intelligence and Healthcare
With the introduction of unprecedented tools for patient care, treatment, and diagnosis, artificial intelligence (AI) is drastically changing the healthcare industry.
For researchers interested in global health, AI-driven health interventions fall into four categories: diagnosis, patient morbidity or mortality risk assessment, disease outbreak prediction and surveillance, and health policy and planning. Machine learning, signal processing, data mining, natural language processing, and other forms of AI are applied in the healthcare sector.
Here are a few current applications of AI in healthcare:
- Diagnosis and treatment: Artificial intelligence (AI) paves the way for the screening of disease and can analyse medical images like X-rays and scans to identify illnesses early and more accurately than humans. AI may be used to create individualised treatment regimens for individuals based on their unique traits and requirements. Other applications of artificial intelligence being used in medicine include Digital chest radiographs, cervical cancer screening, estimating perinatal risk factors, and characterising and predicting the global spread of the Zika virus.
- Drug discovery: Artificial intelligence (AI) may be used to search through extensive databases of chemicals and compounds to find possible new medicines. AI may also be used to foresee how pharmaceuticals would react in the body, lowering the possibility of adverse effects.
- Personalised medicine: Artificial intelligence (AI) may be used to examine a patient’s genetic information, medical history, and lifestyle choices in order to develop a personalised treatment plan that has the highest chance of success.
- Risk assessment: AI may be used to predict the risk of disease and figure out how likely a patient is to have cancer or heart disease. Patients can utilise this knowledge to guide lifestyle adjustments that will lower their risk.
- Healthcare administration: AI may be used to automate processes like appointment scheduling, patient record management, and claim processing. This might free up medical personnel to concentrate on treating patients.
- Telemedicine: Platforms that employ AI in telemedicine can be used to offer doctor consultations via the Internet. Patients with limited access to healthcare in remote locations may particularly benefit from this.
- Robotics: Surgery, pharmaceutical dispensing, and other medical services can be carried out by AI-powered robots. This might aid in enhancing the effectiveness and precision of healthcare delivery.
- Big data analytics: Using AI, enormous databases of healthcare data may be analysed to spot trends and patterns. The diagnosis and treatment of illnesses can be made better with the use of this knowledge.
- Virtual assistants: AI-driven virtual assistants may be used to set up appointments, answer patients’ inquiries, and offer information about their conditions. The patient experience may be enhanced as a result of this.
The future of AI in healthcare is very promising. The use of AI in healthcare is still in its early stages, but it has the potential to revolutionize the way we diagnose, treat, and manage diseases. In the years to come, as AI technology advances, it is anticipated to have a more significant influence on the healthcare industry.
Advances in Gene Editing Technology
The science of gene editing is expanding quickly. The way we treat illnesses is changing as a result of gene editing tools like CRISPR-Cas9. These technologies can be used to fix genetic flaws that lead to disease or to add new genes that can offer disease protection.
The following are some of the developments in gene editing technologies that are being investigated for medical applications:
- CRISPR-Cas9: A protein called Cas9 is used by CRISPR-Cas9 to cut DNA at a precise spot. This enables precise gene replacement, deletion, and insertion. The most popular gene editing technology, CRISPR-Cas9, is being researched for a number of uses, including the treatment of HIV, cystic fibrosis, sickle cell disease, and hereditary illnesses.
For instance, in cancer patients, CRISPR-Cas9 is being utilised to create novel cancer medicines that can target and eliminate cancer cells. CAR T-cell treatments, a sort of immunotherapy that employs a patient’s immune cells to combat cancer, are being developed by researchers utilising CRISPR-Cas9.
- Base editing: A more recent gene editing technique, base editing allows you to alter specific DNA nucleotides without actually cutting the DNA. Compared to CRISPR-Cas9, this makes it less likely to result in unwanted side effects. For the therapy of conditions including cystic fibrosis and Duchenne muscular dystrophy, base editing is being researched.
- RNA editing: An approach to gene editing that can target RNA molecules rather than DNA. This can be utilised to treat conditions like certain cancers that are brought on by RNA alterations.
- Gene therapy: Gene therapy is a treatment that involves introducing genes into cells to correct a genetic defect. Numerous illnesses, including cancer, HIV, and hereditary ailments, have been treated by gene therapy.
These are only a handful of the gene editing innovations that are being investigated for medical applications. Technology’s continued advancement will probably have a significant influence on how we manage diseases in the years to come.
Development of Precision Medicine
A person’s unique genetic makeup, lifestyle, and environment are all taken into consideration when developing a medical treatment plan in precision/personalised medicine. This may result in a more effective and targeted treatment with fewer adverse effects.
Personalising medicine may be done in a variety of ways. Typical strategies include:
- Genetic testing includes examining a person’s DNA to see if there are any mutations or variances that might impact their likelihood of contracting a certain disease or their reaction to a particular medication.
- Biomarkers are quantifiable indications of a biological condition or state. Biomarkers can be used to monitor a patient’s response to therapy or to spot those who are most likely to catch a particular disease.
- Environmental factors, such as pollutant exposure, food, and exercise impact how people respond to therapy as well as the development of many diseases.
Precision medicine is becoming more and more feasible as we understand more about the human genome and the part genetics plays in disease. We can create more effective and focused therapies that may result in improvement by taking into consideration a person’s particular demands.
Here are some examples of current applications of precision medicine:
- High-risk cancer patients are identified via genetic testing, and targeted medicines are created that are more efficient for those who have certain genetic alterations.
- Biomarkers are being utilised to monitor an individual’s risk of developing heart disease and to pinpoint those who will benefit from certain therapies the most.
- Scientists are examining the genetic component of Alzheimer’s disease and creating targeted treatments that might be more efficient for those who carry particular genetic abnormalities.
Some of the challenges and limitations of precision medicine include cost, accuracy, accessibility, and regulation.
Personalised medicine is a promising subject with the potential to enhance millions of people’s lives despite these difficulties. It is anticipated to become more accessible, inexpensive, and accurate as technology advances.
Development of Telemedicine and Remote Healthcare
Telemedicine and remote healthcare allow patients to receive care from a doctor or other healthcare provider without having to travel to a doctor’s office or hospital. This can help with healthcare access, particularly in remote locations. The COVID-19 pandemic has spurred telemedicine and remote healthcare development to a great extent. These services are increasingly enticing to patients and providers alike because of the requirement to maintain social distance and avoid in-person visits to healthcare institutions. There are several advantages to telemedicine and remote medical care, such as better access to healthcare, lower healthcare expenses, increased patient satisfaction, and better patient results.
Remote healthcare services and telemedicine come in a wide variety. The most popular ones are Tele-education, remote patient monitoring, and virtual doctor appointments.
Additionally, there are several drawbacks to telemedicine and remote treatment, such as security and privacy issues, a lack of financing, technical issues, and a shortage of skilled providers.
Despite these impediments, telemedicine and remote healthcare are expanding quickly and playing a bigger role in the healthcare system. These services are expected to become progressively more common and available as technology advances.
Here are some of the future trends in telemedicine and remote healthcare:
- Increasing the use of artificial intelligence (AI): AI may be applied to personalise treatment regimens, increase the precision of diagnoses, and keep track of patient’s health.
- Development of novel telehealth technology: More thorough and individualised treatment will be feasible thanks to new gadgets like wearable sensors and virtual reality headsets.
- Expansion into new areas: Telemedicine and remote healthcare will be utilised to deliver care in new areas, such as managing chronic diseases and mental health.
Application of 3D Printing in Healthcare
3D printing in medicine is being used to create customised medical items including prostheses, implants, and surgical guides. This innovation might save expenditures while raising the standard of treatment. A rapidly developing technology, 3D printing has a wide range of potential uses in the healthcare sector. Among the most widespread applications of 3D printing in the medical field, some are mentioned below:
- Producing patient-specific medical devices: 3D printing may be used to produce personalised medical items like implants, prostheses, and surgical guides that are tailored to the anatomy of a single patient. In addition to lowering the risk of problems, this can enhance the device’s fit and functionality.
- Building medical models and educating healthcare professionals: 3D printing may be used to build accurate representations of the human body’s organs, tissues, and tumours. These models can be used to aid in the planning and execution of intricate treatments as well as the education of patients about their conditions. This can assist them in picking up new abilities and methods, as well as in practising approaches in a secure setting.
- Creating novel medications and treatments: Tissue scaffolds for cell culture and intricate drug delivery systems may be made using 3D printing. This can aid in the development of novel treatments and medications by researchers for a number of disorders.
- Customising care: Using 3D printing, it is possible to develop treatments and drugs that are specifically suited to the requirements of a certain patient. This might increase the therapy’s efficacy and security.
Here are some specific examples of how 3D printing is being used in healthcare today:
- A company named Materialise has created a 3D-printed breast implant that is specifically designed for women with tuberous breasts. This type of breast deformity is often difficult to treat with traditional implants, but the 3D-printed implant can provide a more natural and comfortable fit.
- A team of researchers at the University of California, San Diego has developed a 3D-printed surgical guide that can be used to remove brain tumors with greater precision and accuracy.
- A company named Organovo has developed a 3D printer that can be used to create human tissue. This tissue can be used to study diseases, develop new drugs, and create personalized medical implants.
These are some of the numerous uses for 3D printing that are now being made in the medical field. As technology advances, it will probably have a bigger influence on the healthcare sector, enhancing the standard of treatment and enhancing accessibility for all.
The use of blockchain technology to increase the security and effectiveness of healthcare data exchange is one of the significant developments being made in the world of healthcare. Smart technologies, particularly wearable sensors, are being developed to extract therapeutically significant health-related data from physical (body) indicators like heart rate, blood pressure, body temperature, respiration rate, and body motion. The technology has now also come up with immersive virtual and augmented reality training and education in the medical field.
Advancements in technology, increased investment in global health, partnerships, collaborations among the government, organizations, and individuals, and innovations altogether make a significant contribution to addressing the challenges to global health and improving health outcomes. The rapid pace of technical improvement has made these developments feasible. These technologies will have a bigger influence on global healthcare as they advance.
The Chapter 2 of the NMC Update describes the broad outline of the National Exit Exam, including general features of steps 1 and 2, NExT scores, nature of scores, minimum passing score, etc.
General Features of the NExT Exam
The NExT Exam shall comprise two separate exams referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
NExT Step 1
1.NExT Step 1 shall be a theoretical and Computer-based/Online examination.
2. It shall comprise one or more types of multiple-choice questions.
3. This shall be a Centralized Common All India Examination that will be held by a body designated by the commission as the conducting authority.
4. The examination shall include six papers covering topics from both Part 1 and 2 of the III MBBS/Final MBBS programme:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
(Applied aspects of all subjects covered under I MBBS and II MBBS and Applied aspects of all subjects covered under III MBBS/Final MBBS Part l)
5. Students who have completed their III MBBS/Final MBBS course from a recognized medical college shall be eligible to appear for the examination.
6. NExT Step 1 Examination shall be held twice a year in the months of May and November tentatively.
7. There shall be no restriction on the number of attempts to participate in NExT Step 1 provided that the candidate has completed both the NExT Step 1 and NExT Step 2 exams within ten years of enrolling in the MBBS Course.
8. There is no cap on the number of times for attempting the NExT Step 1 Regular Examination to improve your score but you can only go for the improvement after completing your NExT Step 2.
9. The III MBBS/Final MBBS Part 1 and III MBBS/Final MBBS Part II Practical/clinical examinations will continue to be held conventionally unless otherwise stated by the Commission and the NExT Step 1 will replace the traditional university/institutional Theory Examinations of the III MBBS/Final MBBS Part II.
NExT Step 2
1. The NExT Step 2 shall be a Practical/Clinical and viva voce examination comprising seven clinical subjects/disciplines:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
- Orthopaedics and PMR (Physical Medicine and Rehabilitation)
2. The exam shall be objectively structured, clinical case-based, and use simulated cases and patients to evaluate practical and clinical skills as well as clinical decision-making and communication abilities expected of an Indian medical graduate.
3. The exam must be taken in person or live, and it must be administered by the relevant state health universities or institutions in accordance with the norms and directives given by the Commission. The Commission will choose the university or institution that is permitted to conduct NExT Step 2 for the relevant colleges where there are no state health universities.
4. The Regular NExT Step 2 Exam shall be held twice a year.
5. A NExT Step 2 Supplementary Examination is only open to candidates who have failed in one or more (up to three) of the seven subjects and are required to repeat specific subjects. It will be held twice a year. If a candidate fails in more than three subjects, then they will have to appear in supplementary exams of all the seven subjects.
7. As long as the candidate has completed both the NExT Step 1 and NExT Step 2 Examinations within ten years of enrolling in the MBBS programme, there is no restriction on the number of attempts to participate in NExT Step 2.
NExT Scores
1. Nature of Scoring
- The marks in NExT Step 1 must be calculated as a whole number, which will serve as the Raw Scores with the proper decimals. Also, equivalent Percentages (marks out of a maximum of 100) with the proper decimals may then be calculated.
- The outcomes of the NExT 2 exams will only be reported as Pass/Fail depending on the acquisition of the relevant competence that is being evaluated.
2. Minimum scores for passing
- The minimum score to pass shall be 50% of the total or half of the maximum possible Raw for NExT Step 1.
- To pass the NExT Step 1 exam, you must receive a minimum of 50% (50 out of 100) in each of the six papers or half of the maximum possible Raw Scores.
- The requirements for passing NExT Step 2 include a successful demonstration of having acquired the competencies that are evaluated, with a pass/fail result being given.
3. Calculation of NExT Step 1 scores for determining merit for the purpose of admission to Postgraduate courses in broad specialties
- The sum of the raw scores earned in each paper or topic in a single NExT 1 exam will be used to calculate the Total Marks for determining the merit, particularly for admission to broad specialization Postgraduate Courses.
- The candidate must follow the generation of a rank application process as stipulated by the Commission from time to time in order to determine rank for admission into Postgraduate courses in broad specializations in a given academic year. Only individuals who have submitted an application for rank generation will be eligible for admission for that cycle of the academic year.
- The NExT Step results will be valid for five years in order to determine merit, notably for admission to broad-specialty postgraduate courses. If a candidate has appeared in the NExT exam cycle then the score of the latest given NExT step 1 exam will be considered.
- Tie-breaker rule for rank generation:
-
- Normalized sum of raw scores obtained in each paper in NExT step 1 although the method of normalization will be notified later.
- Candidate with the lower attempts in NExT step 1 will be placed higher in the merit list.
- Candidates will be given higher rank based on the higher marks in the following order of preference:
-
-
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
-
4. Utility of NExT Scores
- An MBBS student from a college recognized by the Commission shall be eligible for compulsory internship only if they pass in each of the six theory papers of NExT Part 1 and also pass in III MBBS/Final MBBS (Part 2) Practical/Clinical Examination.
- A medical student who has completed their undergraduate studies abroad at an institution recognized by the Commission and who has met the necessary requirements outlined in the Commission’s Foreign Medical Graduate Regulations is eligible to participate in the mandatory rotating internship programme only if they pass in all six NExT Step 1 Theory Papers.
- A medical graduate who received their training in India or outside of India will be entitled to register in the Indian Medical Register and State Medical Register and obtain a license to practice modern medicine in India, only if, they have completed the internship for the appropriate length of time and have successfully passed the NExT Step 2 (Practical / Clinical) Examination. You must fulfill all the requirements as per the Registration of Medical Practitioners and Licence to practice Medicine Regulations, of NMC. Also, all the other requirements are considered appropriate by the Commission, Concerned University/Institution and duly applicable at that time.
- For admission to PG medical courses in broad specialty subjects, a candidate must meet the following criteria:
- Candidates must meet the conditions outlined for NExT Part 1 and 2, making them eligible for a license to practice modern medicine in India.
- Must engage in common counselling by a designated authority granted by the Central Government or Commission.
- The NExT Step I Scores may be used by the Government of India, the State Governments, any organization of the Government of India, the State Governments, or any autonomous or private body/institution for the purpose of employment, provided that the necessary authorization has been sought and authorized by the National Medical Commission or other appropriate authorities as determined to be appropriate.
Click Here to Read NMC NExT Exam Update – Chapter 1 (Preliminary)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
The NExT Exam latest news includes Chapter 1 (Preliminary) and Chapter 2 (Broad Outline) and Chapter 3 (General Information).
The core objective of the NExT exam is to provide consistency in summative evaluations conducted across the nation in relation to the minimal requirements for a medical graduate’s education and training.
The National Exit Test (NExT), shall serve as a licentiate examination for validating a medical graduate’s eligibility to register for practice the contemporary system of medicine in India.
NExT will also act as an entrance exam for admission to PG medical education in broad medical specialties by determining the eligibility and ranking of the MBBS students.
The National Exit Exam shall be applicable to:
- All undergraduate medical students seeking the MBBS degree at all medical colleges that have been accredited by the National Medical Commission along with Institutes of National Importance (INIs) are subject to the National Exit Test (NExT).
- All foreign medical graduates who have been granted approval by the NMC for the purposes of obtaining a license to practice medicine as a registered medical practitioner in India and for enrollment in the State Register or the National Register in such a manner as may be specified by regulations.
- Anyone with a medical degree aiming to pursue an academic course, an observership, or any other purpose that may be specified and allowed by the NMC by appropriate notification or rules from time to time.
- Anyone with the granted medical license practicing in India wishes to pursue PG degree can take the NExT exam.
According to the draft released, the NExT comprises two separate examinations, referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
The Commission shall from time to time determine, by appropriate regulations and/or notification, the applicable method of employing the NExT results for admission to Postgraduate Courses in wide medical specialties by means of common counselling by the designated authority.
There is no confirmation yet on the academic session to which the NExT exam will be applicable but when it will come into force, all other corresponding and equivalent examinations shall be phased/ceased out.
It is still to be decided by the Commission Central Government, State Government, that the existing examinations, however, shall continue for as long as may be necessary or the analogous existing exams will be replaced by the NExT. The Commission will decide when it is necessary and will notify the use of scores and normalization of various examinations and the NExT, when applicable concurrently, for such purposes as may be appropriate.
Chapters 2 and 3 of the update include the complete structure of the NExT Examination, objectives, exam pattern, eligibility, distribution of subjects, nature of scoring, timetables, and more.
Click Here to Read NMC NExT Exam Update – Chapter 2 (Broad Outline)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
The Membership of the Royal College of Physicians (MRCP) is a postgraduate diploma in internal medicine in the United Kingdom. It’s a valuable qualification as it’s an internationally recognized diploma and is the shortest route to a career in medicine around the world. The exam tests students on their knowledge of basic medical sciences as well as the clinical skills required for the diagnosis and management of diseases. The MRCP is recognized in countries around the world, and valued especially in the UK, the UAE, Singapore, and Ireland. The MRCP is also recognised by UAE’s board and opens up opportunities to practice in the Middle East as well.
The MRCP is challenging and preparing for it takes months, since students usually take it while pursuing their post-graduation, but the advantages of obtaining a MRCP degree makes the pressure worthwhile. You cannot sit the MRCP exam without having completed 12 months of medical experience by the date of the examination, as the MRCP focuses on the real world applications of medical knowledge, measuring not just your theoretical knowledge, but your practical skills as well. It is designed to test your competence in medicine overall.
Once you have the certification, you can work as a consultant physician in a private hospital in India. However, another advantage of passing the MRCP medical exam is its recognition abroad.
All you need to know about MRCP Examination & MRCP Full Form
MRCP is the Membership of the Royal Colleges of Physicians of the United Kingdom. The exam is conducted for doctors who are interested in receiving higher specialty training from the Royal College of Physicians of Edinburgh, the Royal College of Physicians and Surgeons of Glasgow, and the Royal College of Physicians of London. It is a set of three exams designed to test the knowledge, skills, and behavior of clinicians in training.
MRCP(UK) is conducted in three parts:
- MRCP Part 1 (Written Examination)
- MRCP Part 2 (Written Examination)
- MRCP Part 2 Clinical Examination (PACES)
MRCP (UK) studies play an important role in the overall educational experience and continuing professional development of doctors in the UK and internationally. An MRCP (UK) Diploma is required for doctors who wish to undergo training in the medical specialty in the United Kingdom. The MRCP exam is a globally recognized qualification that is seen as an excellent benchmark against which doctors are judged on their competence and suitability for specialist training.
How to apply for the MRCP exam 2023?
- Register online through My MRCP (UK) official website.
- Make sure to recheck all the details you have mentioned.
- At this point, you will be required to submit evidence of primary medical qualification (PMQ).
- After the basic registration, go to the Upcoming exams section and apply for the respective exam type you want to appear for (Part 1/2/PACES).
- Mention the details if you are training in UK or not.
- Choose a country and city as your examination center.
- Fill out the details in the special arrangement section if required.
- Pay the applicable examination fee.
- Your application is confirmed via an automatically generated email.
- Candidates who have limitations in their practice should fill out an online declaration form with the application itself.
Mode of MRCP Exam
The exam is conducted in two modes:
- Online mode: The exam is conducted in online mode using an online proctored system for candidates within the UK and the Republic of Ireland. The students appearing for the online exam will have to fulfill all the criteria as per the organization and read the guidelines including the online exam procedure, IT setup, important points to know before and after the exam, and other exam regulations and codes of conduct.
- Offline mode: The rest of the candidates from different countries including India will have to give the exam in the offline mode. Offline exams are conducted at exam centers in various countries. However, the exam center is different for the MRCP Exam part 1 & 2 and PACES.
The content and format of the exam are the same for both modes so the preparation should be done in the same way.
Read out further to get the complete information about all the three parts of the MRCP exam.
MRCP Part 1
Aim of MRCP Exam Part 1
- It is an entry-level exam.
- The purpose of the MRCP Part 1 is to test the understanding of basic clinical sciences that a medical graduate is expected to comprehend.
- Part 1 exam is designed to assess students’ knowledge of clinical science and prevalent and significant illnesses as described in the UK curriculum.
- Additionally, you’re tested on the most important and commonly encountered diseases from several specialties.
MRCP Exam Eligibility
Medicos from any part of the world can give the exam. Candidates with a medical degree from an institute recognized by GMC (General Medicine Council), followed by 12 months of medical employment after your graduation are eligible to apply for the exam.
Candidates are required to send proof/evidence of completion of their medical degree along with at least 12 months of medical employment.
MRCP Part 1 Exam Dates
MRCP 1 is conducted 4 times a year. The 2022/4 exam will be held on 30th Nov 2022 and the result will be declared on 11th January 2023.
Exam Schedule for MRCP Part 1 Exam 2023
| 2023 Session | Application Period | Exam Date | Result Date |
| 1st (2023/1) |
7 Nov 2022 – 14 Nov 2022 | 25 Jan 2023 | 8 Mar 2023 |
| 2nd (2023/2) |
13 Feb 2023 – 20 Feb 2023 | 19 Apr 2023 | 31 May 2023 |
| 3rd (2023/3) |
29 May 2023 – 5 Jun 2023 | 9 Aug 2023 | 13 Sep 2023 |
| 4th (2023/4) |
14 Aug 2023 – 21 Aug 2023 | 18 Oct 2023 | 29 Nov 2023 |
MRCP Part 1 Exam fees
- For part 1, the examination fee is £460 for UK students.
- For international students including India, the exam fee is £616, which approximately amounts to 59,904.20 Indian Rupee. The amount in INR can vary depending on the currency difference.
MRCP Part 1 Exam Pattern
- It is a single-day examination.
- It consists of two papers of 3 hours duration each.
- Each paper has 100 questions.
- MCQ pattern with the ‘best of five options’ type questions.
- There is no negative marking.
- There are no image-based questions.
Subject weightage in MRCP Part 1
The exam comprises questions from the various specialties:
| Specialty | Number of questions |
| Cardiology | 14 |
| Clinical Pharmacology and Therapeutics | 15 |
| Clinical Sciences | 25 |
| Dermatology | 8 |
| Endocrinology, diabetes and metabolic medicine | 14 |
| Gastroenterology and Hepatology | 14 |
| Geriatric medicine | 8 |
| Hematology | 10 |
| Infectious diseases | 14 |
| Neurology | 14 |
| Oncology | 5 |
| Medical ophthalmology | 4 |
| Palliative medicine and end of lifecare | 4 |
| Psychiatry | 9 |
| Renal medicine | 14 |
| Respiratory medicine | 14 |
| Rheumatology | 14 |
| TOTAL – 200 |
The Clinical Sciences portion will include questions from the following specialties:
| Specialty | Number of questions |
| Cell, molecular, and membrane biology | 2 |
| Clinical anatomy | 3 |
| Clinical biochemistry and metabolism | 4 |
| Clinical physiology | 4 |
| Genetics | 3 |
| Immunology | 4 |
| Statistics, epidemiology, and evidence-based medicine | 5 |
Marking System for Part 1 and Part 2 Written Examination
An “Equating method” is used for calculating a candidate’s overall score. This procedure is statistically based on item response theory and utilized to guarantee equivalent outcomes for candidates in the test for equivalent performance on various diets.
All candidates are given an “overall scaled score” instead of an overall percentage score. The grade is calculated based on the number of questions answered correctly in the two test papers of the exam and takes into account the relative difficulty of the exam.
Note:
- For every correct response, a +1 mark is awarded.
- There is no negative marking in the MRCP written exam.
- If a candidate opts for more than one correct response or the answer is not correctly marked, then the marks awarded to the candidate are zero.
Passing Marks
As per the last academic session, the qualifying score for MRCP Part 1 exam is 540 marks. You need to get at least these many marks to qualify for MRCP Part 1 and become eligible for the MRCP part 2 written exam.
MRCP Part 2
Aim of MRCP Exam Part 2
In this exam, the capacity of the doctors to use clinical knowledge, form clinical judgments, and assume accountability will be evaluated.
Factors evaluated in MRCP Part 2:
- Putting issue or diagnostic lists to prepare an investigation
- Choosing a strategy for emergency management
- Choosing a long-term management strategy
- Determining prognosis
MRCP Part 2 Eligibility
To be eligible for Part 2, the candidate must have successfully passed the MRCP Part 1 written exam within the preceding 7 years.
A candidate will have to re-appear for the Part 1 written exam if he/she could not pass the MRCP Part 2 written or PACES exam within 7 years of passing the MRCP part 1 exam.
MRCP Part 2 Exam Dates
The MRCP exam is also conducted 4 times a year. The 2022/4 part 2 exam will be held on 14th December 2022 and the result will be declared on 25th January 2023.
Exam Schedule for MRCP Part 2 Exam 2023
| 2023 Session | Application Period | Exam Date | Result Date |
| 1st (2023/1) |
21 Nov 2022 – 28 Nov 2022 | 22 Feb 2023 | 05 Apr 2023 |
| 2nd (2023/2) |
13 Mar 2023 – 20 Mar 2023 | 17 May 2023 | 28 Jun 2023 |
| 3rd (2023/3) |
03 Jul 2023 – 10 Jul 2023 | 06 Sep 2023 | 18 Oct 2023 |
| 4th (2023/4) |
18 Sep 2023 – 25 Sep 2023 | 22 Nov 2023 | 03 Jan 2024 |
MRCP Part 2 Exam fees
- For UK students, the examination fee is £460.
- For international students including India, the exam fee is £616, which approximately amounts to 59,904.20 Indian Rupee. The amount in INR can vary depending on the currency difference.
MRCP Part 2 Exam Pattern
- It is a single-day examination.
- It consists of two papers of 3 hours duration each.
- Each paper has 100 questions.
- MCQ pattern with the ‘best of five options (BOFs)’ type questions.
- There is no negative marking.
- These include image-based questions, unlike Part 1.
Subject weightage in MRCP Part 2
For the theoretical questions, you can expect the following pattern of distribution
| Specialty | Number of questions |
| Cardiology | 19 |
| Clinical Pharmacology and Therapeutics | 18 |
| Dermatology | 9 |
| Endocrinology, diabetes and metabolic medicine | 19 |
| Gastroenterology and Hepatology | 19 |
| Geriatric medicine | 9 |
| Haematology | 9 |
| Haematology | 10 |
| Infectious diseases | 19 |
| Neurology | 17 |
| Oncology | 6 |
| Medical ophthalmology | 3 |
| Palliative medicine and end of lifecare | 3 |
| Psychiatry | 3 |
| Renal medicine | 19 |
| Respiratory medicine | 19 |
| Rheumatology | 19 |
| TOTAL – 200 |
For the image-based questions, you can expect questions from:
- Clinical photographs
- Pathology slides
- Inheritance trees
- ECGS
- X-rays
- CT and MR scans
- Echocardiograms
In the Part 2 exam, the questions are usually based on clinical scenarios and may be illustrated images. There can be questions related to the diagnosis, investigation, management, and prognosis of patients.
Passing marks
454 marks are considered a qualifying score for part 2. After you have cleared your MRCP part 2, you can proceed toward your MRCP Part 2 Clinical Examinations, i.e., PACES.
The MRCP Part 1 and Part 2 examination are both written exams and have almost the same pattern, but the PACES exam is entirely different from both parts. It has a completely different pattern and evaluation procedure.
MRCP Part 2 Clinical Examination (PACES)
PACES, abbreviated for Practical Assessment of Clinical Examination Skills, is designed to examine the clinical knowledge and acumen of doctors who wish to enter advanced training (ST3).
Aim of the PACES Exam
You are desired to know each of the following clinical skills:
- Clinical examination
- Identifying physical signs
- Clinical communication
- Differential diagnosis
- Clinical judgment
- Managing patient concern
- Maintaining patient welfare
Eligibility for MRCP PACES
The eligibility for PACES is the same as is for MRCP 2, i.e, you must have cleared your MRCP part 1 within the last 7 years.
MRCP PACES Exam Date
It is conducted 3 times a year, from January to March, June to August, and September to December.
The dates for the PACES exam are different for the UK and other countries and even for different centers.
MRCP PACES Exam Pattern
It is a half-day examination that takes place at hospitals or clinical centers.
There are five clinical positions (Stations) staffed either by patients with a specific disease or by trained support staff (surrogates). Each station has two independent examiners who observe and evaluate the candidates’ performance.
You can start at any station and move to the next station every 20 minutes until you complete the cycle. There is a 5-minute break between each station.
The five stations are allotted for the following:
- Respiratory, Abdomen
- History taking
- Cardiovascular and Nervous system
- Communication skills
- Brief clinical consolation
At least 4 weeks before your examination date, admission documents with your assigned examination date, time, and location will be sent.
Application Process
All the candidates are advised to read all the instructions carefully before filling out the application form.
2023 Application dates for the UK
| 2023 Session | Application Period | Assessment Period |
| 1st (2023/1) |
14 Nov 2022 – 21 Nov 2022 | Late January – March |
| 2nd (2023/2) |
27 Mar 2023 – 03 Apr 2023 | Early June – Early August |
| 3rd (2023/3) |
24 Jul 2023 – 31 Jul 2023 | Late September – Early December |
2023 International Application Period
| 2023 Session | Application Period |
| 1st (2023/1) |
10 Oct 2022 – 17 Oct 2022 |
| 2nd (2023/2) |
20 Feb 2023 – 27 Feb 2023 |
| 3rd (2023/3) |
19 Jun 2023 – 26 Jun 2023 |
In the 2023 International Application Period, the assessment period is not yet released.
Exams are not scheduled for each day of the assessment period, and exam schedules differ amongst colleges. Your exam date and venue will be listed in your admissions application.
MRCP PACES Fees
- For UK students, the examination fee is £657.
- For international students including India, the exam fee is £1202, which approximately amounts to 1,16,891.00 Indian Rupee. The amount in INR can vary depending on the currency difference.
Marking System for MRCP Part 2 Clinical Examination (PACES)
The candidates are assessed based on their clinical skills in this part of the exam. The exam process is as follows:
- Five clinical stations are set up with either trained stand-ins or patients with a specific disease (surrogate patients).
- There are two separate examiners at each station.
- For prospects to succeed, the candidate must achieve a minimum standard in each of the seven competencies as well as a minimum overall score.
Passing marks in PACES
You need to pass each clinical station separately based on clinical standards. Additionally, a minimum of 130 out of 170 is required to pass the PACES.
Let’s read some relevant information for all the parts of MRCP.
Number of attempts for the MRCP Exam
A maximum of six attempts are allowed at each part of the MRCP (UK) diploma. If any candidate wants to appear after six attempts, then for each re-exam, they must have undertaken additional educational experience. A candidate will also have to submit a form along with evidence of the additional educational experience, supported by the candidate’s Educational Supervisor and the Training Programme Director or equivalent.
MRCP Exam Centre
MRCP (UK) exams can be taken anywhere in the world. Candidates have the option of giving MRCP (UK) written exams at 34 international locations and the MRCP (UK) Clinical Examination (PACES) at 16 different locations.
MRCP Exam Centre in India
For Parts 1 and 2:
- Chennai
- Hyderabad
- Kerala
- Kolkata
- Mumbai
- New Delhi
For PACES:
- Bengaluru
- Chennai
- Hyderabad
- Kochi
- Kolkata
- New Delhi
- Pondicherry
- Thiruvananthapuram
Language requirements
- The MRCP exam (all parts) is conducted in English language only.
- The candidates are advised to have a command of the English language equivalent to a 7.5 band score in the IELTS exam. However, no language exam is required to be eligible for the MRCP exam.
Examining Board
There are examination boards for the MRCP (UK) Part 1, MRCP (UK) Part 2 Written, and MRCP (UK) Part 2 Clinical (PACES) exams. The examining board for PACES is also referred to as the Clinical Examining Board (CEB). Its task is to ensure the scientific quality of the examinations, which includes approving the content and determining the passing grade. The examination boards also deal with appeals, cases of scientific or professional misconduct, and complaints.
Withdrawal and Refund
Any candidate who wishes to withdraw his/her application should contact the appropriate administrative office by email and complete all the withdrawal procedures. They must mention the following details in the email for identity verification such as RCP code number, full name, and date of birth. The withdrawal application will not be counted as an attempt.
The withdrawal request must be submitted before the application process ends, so that a refund of 90% can be generated. A 10% application fee is deducted as an administrative charge.
Completion of MRCP Diploma
Once a candidate completes the last component of the diploma successfully, a results letter that attests to their success is given. Details about membership elections and entrance ceremonies is included in this email.
Right time to take your MRCP Exam
In general, data suggests that candidates have the highest pass rates when the candidates
- take the first part 1 exam attempt within 12-24 months of graduation
- take the first part 2 exam attempt within 36 months of graduation
- take the first part 2 clinical exam (PACES) attempt at least after 36 months of graduation
- Pass the Part 2 written exam before taking PACES.
- Before applying for PACES and completing the exam, it is advised to at least have 2 years of core medical training experience. A candidate should involve in emergency medical patient care for at least 4 months in the 2-year tenure of medical practice.
The information here will help you make the best choice about when to take the exam.
Points to note:
- Candidates are not allowed to apply through any third-party organization.
- After passing Part 1, candidates are ineligible to retake the exam until the 7-year window is passed.
- A candidate must complete both Part-2 written and clinical within seven years after the MRCP part 1 exam.
- A candidate is advised to attempt the mock test available on the MRCP UK official website.
- Before taking any of the examinations, candidates are highly encouraged to become familiar with the contents of these publications:
- MRCP (UK) Regulations (updated August 2022)
- Specialty Certificate Examination Regulations
- European Specialty Examination Regulations
- Examination Appeals Regulations
- Examination Complaint Procedure
- Reasonable Adjustments Procedure
- Code of Conduct
- Misconduct Regulations
If you want the opportunity of working abroad in the UK, the Middle East, Australia, Singapore, and many other countries, then the MRCP is the best qualification to have. The MRCP is a prerequisite to anyone wishing to go on to a specialist training post as a physician in the United Kingdom and in Australia. In the UAE, the MRCP is considered a super speciality degree, and consequently, those who have taken the MRCP are paid at par with super specialists. Doctors who pass the MRCP Exam can apply to jobs in any country that recognizes the degree abroad. Most countries welcome people who have professional degrees and can add value to the country and help its citizens. If you’re a doctor, you have a higher chance of being granted a work visa than most other jobs. If you think at some point you may want to live abroad, the MRCP is by far the best qualification to have.
DigiNerve is an e-learning platform by Jaypee which offers information and online coaching courses for the MRCP exams.
Frequently Asked Questions (FAQs)
-
Is there any online course for preparation for MRCP Part 1?
Ans: For cracking your MRCP 1, you have the strongest preparation available on DigiNerve, prepared by the eminent faculty of medicine, Dr. Archith Boloor and Dr. Gurpreet Singh Wander. The course is based on The Royal College of Physicians’ curriculum (RCP). There are 15 online modules in the course, which includes content on major disciplines including Clinical Sciences, Cardiology, Gastroenterology, etc. It also includes high-yield questions, mock papers, e-chapters, video lectures, notes and BOFs.
-
How many stages does MRCP has?
Ans: It is a set of 3 exams designed to test the knowledge, skills, and behavior of clinicians in training.
- MRCP Part 1 Written Examination
- MRCP Part 2 Written Examination
- MRCP Part 2 Clinical Examination (PACES)
-
How much is the MRCP exam fees?
Ans: The fees for MRCP Part 1 and 2 (Written):
- £460 (UK)
- £616 (International)
The fees for MRCP Part 2 Clinical Examination (PACES):
- £657 (UK)
- £1202 (International)
-
How many attempts do you get at MRCP?
Ans: A maximum of six attempts are allowed for each part of the MRCP (UK) diploma. If any candidate wants to appear after six attempts, then for each re-exam, they must have undertaken additional educational experience.
INI-CET is a combined national-level entrance examination for admission to the medical postgraduate courses – MD, MS, DM (6 yrs), MCh (6 yrs), and MDS at INI institutes (Institute of National Importance). The INI-CET January session 2023 exam is around the corner. Getting admission to INI institutes is highly challenging and a dream for MBBS students. This is a highly competitive task to secure a seat in the renowned medical colleges in India.
Remember, Perseverance is the key.
The INI-CET exam is going to be held on 13th Nov 2022 for admission to the AIIMS INI-CET January session 2023.
Mode and Scheme of INI-CET January 2023 exam
| Particulars | Description |
| Mode of Examination | Computer-based test (CBT) |
| Duration | 3 hours (180 minutes) |
| Number of questions | 200 |
| Types of questions | Objective type |
| Marking Scheme | +1 mark for every correct response and -1/3 for every incorrect response |
Important things to know:
- If more than one candidate scores the same, then this tie-breaker situation is resolved by applying the following criteria sequentially:
-
- Less negative marks
- Older by age
- Candidates equal to 8 (eight) times the number of postgraduate seats available in each category will be called for the first and second rounds of seat distribution based on the INI-CET merit list.
- Spot Round Counseling will only be conducted if the seats will remain vacant even after the open round counseling.
List of Participating Institutes for INI-CET January 2023 Session
| S. No. | Name |
| 1 | AIIMS, New Delhi |
| 2 | AIIMS, Bhopal |
| 3 | AIIMS, Bhubaneswar |
| 4 | AIIMS, Jodhpur |
| 5 | AIIMS, Nagpur |
| 6 | AIIMS, Patna |
| 7 | AIIMS, Raipur |
| 8 | AIIMS, Rishikesh |
| 9 | AIIMS, Bibinagar |
| 10 | AIIMS, Bhatinda |
| 11 | AIIMS, Deoghar |
| 12 | AIIMS, Mangalagiri |
| 13 | AIIMS, Raebareli |
| 14 | JIPMER, Puducherry |
| 15 | NIMHANS, Bengaluru |
| 16 | PGIMER, Chandigarh |
| 17 | SCTIMST, Trivandrum |
Here’s the tentative seat distribution (Category-wise) for admission to various MS/MD/DM (6 years)/MCh (6 years)/MDS courses at AIIMS, New Delhi and other 12 AIIMS through the INI-CET entrance examination for the January session of 2023.
Table 1: Tentative seat distribution for INI-CET January 2023 session at AIIMS, New Delhi:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 17 | 7 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Biochemistry | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Biophysics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Community Medicine | 9 | 5 | 2 | 1 | 0 | 1 |
| MD | Dermatology & Venerology | 5 | 1 | 2 | 1 | 0 | 1 |
| MD | Emergency Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Geriatric Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Lab. Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Medicine | 11 | 5 | 3 | 2 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 4 | 3 | 0 | 0 | 0 | 1 |
| MD | Obstetrics & Gynecology | 11 | 4 | 3 | 2 | 1 | 1 |
| MD | Ophthalmology | 6 | 3 | 1 | 1 | 1 | 0 |
| MS | Orthopaedics | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Otorhinolaryngology | 5 | 1 | 1 | 1 | 1 | 1 |
| MD | Pediatrics | 10 | 3 | 3 | 2 | 1 | 1 |
| MD | Palliative Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Pathology | 10 | 4 | 3 | 1 | 1 | 1 |
| MD | Pharmacology | 6 | 1 | 2 | 1 | 1 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Physiology | 10 | 5 | 2 | 1 | 1 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Radiodiagnosis & Internventional Radiology | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiation Oncology | 4 | 3 | 1 | 0 | 0 | 0 |
| MS | Surgery | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Transfusion Medicine | 5 | 2 | 2 | 1 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MDS | Pediatrics & Preventive Dentistry | 2 | 0 | 1 | 0 | 0 | 1 |
| MDS | Prosthodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MCh | Neuro Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Paediatric Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Infectious Diseases DM(Direct 6 year Course) | 4 | 4 | 0 | 0 | 0 | 0 |
Table 2: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhopal:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 1 | 0 | 1 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynecology | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Ophthalmology | 3 | 1 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | Pathology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 0 | 0 | 1 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine & Blood Bank | 2 | 0 | 0 | 1 | 1 | 0 |
Table 3: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhubaneswar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 9 | 3 | 2 | 2 | 1 | 1 |
| MD | Anatomy | 7 | 3 | 2 | 2 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Dermatology | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Emergency Medicine | 5 | 2 | 1 | 1 | 1 | 0 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | General Medicine | 3 | 2 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Obst. & Gynecology | 6 | 3 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 6 | 4 | 1 | 0 | 0 | 1 |
| MD | Pediatrics | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Pathology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Physiology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | PMR | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 0 | 1 | 1 | 1 |
| MD | Radiodiagnosis | 3 | 2 | 0 | 0 | 1 | 0 |
| MD | Radiotherapy | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Transfusion Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
Table 4: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Jodhpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology & Critical Care | 17 | 6 | 5 | 3 | 1 | 2 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Community Medicine | 6 | 2 | 2 | 1 | 1 | 0 |
| MD | Dermatology & Venerology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Emergency Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | General Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | General Surgery | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Microbiology | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | Otorhinolaryngology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | Paediatrics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Pathology | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physiology | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | PMR | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Radiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Transfusion Medicine & Blood Bank | 2 | 1 | 1 | 0 | 0 | 0 |
| MCh | Paediatric Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Radiation Oncology (D.M. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
Table 5: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Patna:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 18 | 8 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 3 | 1 | 0 | 1 | 0 |
| MD | Biochemistry | 9 | 4 | 3 | 2 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 8 | 3 | 2 | 1 | 0 | 2 |
| MD | Dermatology | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | ENT | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Emergency Medicine | 7 | 2 | 2 | 2 | 0 | 1 |
| MD | FMT (Forensic Medicine & Toxicology) | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Medicine | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | OBG (Obstetrics & Gynaecology) | 5 | 1 | 1 | 0 | 2 | 1 |
| MD | Ophthalmology | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Orthopaedics | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Pediatrics | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pathology | 5 | 0 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 3 | 0 | 0 | 0 | 0 |
| MD | Physiology | 7 | 4 | 2 | 1 | 0 | 0 |
| MD | PMR | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Radiodiagnosis | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiotherapy | 2 | 0 | 2 | 0 | 0 | 0 |
| MS | Surgery | 5 | 2 | 1 | 1 | 0 | 1 |
| MCh | Pediatric Surgery (MCh 6 Years) | 3 | 3 | 0 | 0 | 0 | 0 |
Table 6: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raipur:
| Course | Subject/Specialty | Total Number of seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 13 | 4 | 4 | 2 | 1 | 2 |
| MD | Anatomy | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Community Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Dermatology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Emergency Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MS | ENT | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 9 | 4 | 3 | 1 | 0 | 1 |
| MS | General Surgery | 8 | 3 | 3 | 1 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 7 | 2 | 1 | 2 | 0 | 2 |
| MD | Ophthalmology | 8 | 4 | 2 | 1 | 1 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pediatrics | 7 | 3 | 1 | 1 | 1 | 1 |
| MD | Pathology | 8 | 4 | 2 | 2 | 0 | 0 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physical Medicine & Rehabilitation | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Physiology | 2 | 0 | 1 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 1 | 0 | 0 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Pediatric and Preventive Dentistry (MDS) | 1 | 0 | 1 | 0 | 0 | 0 |
Table 7: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Rishikesh:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 7 | 3 | 2 | 1 | 0 | 1 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 2 | 0 | 0 | 1 | 1 |
| MD | Community & Family Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Dermatology & Venerology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Emergency Medicine | 3 | 2 | 0 | 1 | 0 | 0 |
| MS | ENT | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Geriatric Medicine | 1 | 0 | 1 | 0 | 0 | 0 |
| MS | General Surgery | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Nuclear Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Ophthalmology | 6 | 4 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pathology | 5 | 3 | 1 | 1 | 0 | 0 |
| MD | Pharmacology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Physiology | 3 | 2 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiation Oncology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Respiratory Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MDS | Periodontics (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MCH 6 Years | Pediatric Surgery (MCH 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Plastic, Reconstructive & Burns Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Neurosurgery (MCH 6 yrs) | 1 | 1 | 0 | 0 | 0 | 0 |
Table 8: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Nagpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine | 3 | 1 | 2 | 0 | 0 | 0 |
| MD | Dermatology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 0 | 2 | 0 | 0 | 1 |
| MS | General Surgery | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Ophthalmology | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Otorhinolaryngology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Pediatrics | 3 | 0 | 1 | 0 | 1 | 1 |
| MD | Pathology | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics (MDS) | 0
|
0 | 0 | 0 | 0 | 0 |
Table 9: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bibinagar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | FMT | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 2 | 1 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Peediatrics | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Pathology | 2 | 1 | 0 | 0 | 0 | 1 |
Table 10: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bathinda:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Ophthalmology | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 0 | 1 | 0 | 0 | 0 |
Table 11: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Deoghar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | FMT | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Pathology | 1 | 1 | 0 | 0 | 0 | 0 |
Table 12: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Mangalagiri:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Table 13: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raebareli:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Last-Minute Tips for INI-CET Exam:
- Candidates must carry all the asked documents such as INI-CET admit card, passport size photograph, valid photo ID proof, and a copy of MCI registration certificate with them on the exam day.
- Reverify all your documents before coming to the exam hall.
- Candidates are advised to go through all the guidelines issued by AIIMS for the examination.
- Candidates must reach the INI-CET exam center before time to avoid any chaos.
- Avoid Stress and be confident.
- Eat healthy and sleep well.
- Time management is a must before and during the exam.
To get conceptual clarity on the MBBS courses online, click here
The National Medical Commission (Undergraduate Medical Education Board) has issued new guidelines and the academic calendar for MBBS 2022-2023 batch on 12th Oct 2022.
As per the new NMC guidelines, the classes for the first-year MBBS batch will start on 15th Nov 2022.
Academic Calendar for the 2022-2023 MBBS Batch
According to the new NMC guidelines, there is a change in the academic calendar of MBBS 2022-2023. However, the duration of the MBBS course is the same i.e., 5.5 years including a one-year rotational internship.
| Professional Year | Time Frame | Subjects | Months(Teaching + Exam + Results) |
| 1st | 15th Nov’22 to 15th Dec’23 | Anatomy, Physiology, Biochemistry | 13 months |
| 2nd | 16th Dec’23 to 15th Jan’25 | Pathology, Microbiology, and Pharmacology | 13 months |
| 3rd (III-part-1) | 16th Jan’25 to 30th Nov’25 | Forensic Medicine and Toxicology, Community Medicine/PSM | 10.5 months |
| 4th (III-part-2) | Dec’25 to May’27 | General Surgery, General Medicine, Pediatrics, Obstetrics & Gynecology, ENT, Ophthalmology |
17.5 months |
| Internship | 1st Jun’27 to 31st May’28 | As per the CRMI 2021 Regulations | 12 months |
| PG | 1st Jul ‘28 |
For the academic year 2022-2023, the one-year compulsory rotational internship will start from the 1st June 2027 and end on 31st May 2028, as per the CRMI 2021 regulations.
The following guidelines have been issued by the NMC for the 2022-23 MBBS batch:
- The MBBS batch will commence on 15th Nov 2022.
- The college vacations and examination schedules may be notified as per the affiliated universities of the respective colleges.
Other board guidelines are as follows:
- Regarding Electives – 2 blocks of 15 days each are to be adjusted by the colleges for
- Pre/para-clinical branches
- Clinical branches
- In the 2022-2023 academic batch, the supplementary exams will be conducted with a gap of 1 month from the regular exams and the results will be declared within 15 days.
- There shall be no supplementary MBBS batches.
- The remaining rules and regulations shall remain the same as per the GMER (Graduate Medical Education Regulations) 1997. You can visit the site for GMER 1997 details: https://www.nmc.org.in/rules-regulations/graduate-medical-education-regulations-1997/
- The Yoga and Family Adoption Program through village outreach shall continue for the 2021-2022 MBBS Batch.
Along with the changes in the curriculum and the guidelines mentioned above, a few more notifications have been issued by the NMC from the 2022 batch:
- The NMC has created an Anti-Ragging Committee and Dr. Aruna V. Vanikar, President, UGMEB has been appointed as the chairperson of the committee.
- In the NMC notification stated on 4 Oct 2022, the implementation of HMIS (Hospital Management Information System) is mandated in all medical colleges.
- The NEET UG counselling link is active from 11th Oct 2022 on the MCC official website: https://mcc.nic.in.
Click here to read about the NMC NExT Exam update 2023 including the guidelines, complete structure, exam dates and more.
COVID-19 has devastated families, institutions, and livelihoods while also scarring those at the front lines who witness it every single day. The strain put on our mental health during COVID-19 cannot be understated and the lockdown spent watching the news during such a time of extreme crisis has pressured our mental health further. It can be helpful to take moments out of your day to truly reflect on COVID-19’s impact on education and the mental health of students that might be fractured at the moment.
For those looking to pursue medicine, seeing crippling amounts of pressure being put on the healthcare system might be personally worrying. However, it is especially important to consider the mental health of students at such a critical juncture. To help take care of your mental health during covid-19, keep the following tips in mind to reduce stress.
- Free Headspace Subscription – Headspace is a US-based meditation app that announced a free subscription to all healthcare workers in India to tackle their mental health during COVID-19. Headspace has conducted numerous studies to reach the definitive conclusion that with just 30 days of guided meditation and practicing mindfulness, there has been a 30% stress reduction, greatly boosting mental health of students during COVID-19. If you are searching for a sense of peace in your days, consider signing up for Headspace.
- Take Care of Your Health – It can be difficult to separate your own life from those you care for but finding time to ensure that you are getting the exercise and nutrition you need is essential for myriad reasons. Firstly, an adequate diet that is supplemented with vitamins and nutritious food is essential to building up your immune system, an important factor when amid a pandemic. Secondly, as physical and mental health during covid-19 are interrelated, exercise regularly, try and sleep for full 8 hours, and eat healthy.
- Communicate Often – One of the best ways to destress and find a connection in an isolating time is to talk to other people. Be it friends, family, or a counselor, consider finding a connection and a way to unwind. Especially when considering COVID-19’s impact on the education and mental health of students during covid-19, these forms of socialization may provide a much-needed respite.
- Limit News – The endlessness of social media coupled with the stress of news can seriously harm the mental health of students during covid-19 and adults alike. While we all must remain alert about further developments in the pandemic, limit the amount of time that you ingest news.
If you find moments of solace through submerging yourself into challenging but rewarding tasks, perhaps signing up for an online course is a good way to spend your day. To get started, click here to view DigiNerve’s medical course options.
The Membership of the Royal Colleges of Physicians (MRCP) is a postgraduate medical degree by the United Kingdom that can be obtained through a three-part medical entrance exam. Being highly competitive, acing it requires mentoring and study guides. The MRCP exam has much allure, including prestige, international recognition, and boosting your CV but first students need to understand the basics of what the MRCP exam is, and what the three parts entail-
MRCP Part 1 – MRCP Part 1 is a written exam that involves two papers, each one is 3 hours long and contains 100 best of fives (BOF) questions. To crack the MRCP Part 1, detailed and consistent preparation is the key to the first attempt of success.
MRCP Part 2 (Written Exam) – The Part 2 course follows the same format as the MRCP part 1 exam structure and cracking it will take the same sincere preparation.
MRCP Part 2 (Clinical Paces Exam) – The clinical paces course is the last part of the MRCP exam and is the practical assessment of critical examination skills. It is conducted by two senior physicians as independent examiners who will observe and evaluate each student’s practical skills.
Now that you know the basic format of the MRCP exam, the question needs to be asked – why should you choose an MRCP degree?
- Recognition Abroad – While India recognises the MRCP degree as being equivalent to other postgraduate degrees, it has even more benefits if you plan to work outside of India. Due to its wide recognition and prestige, an MRCP degree holder has a significant advantage over other medical degrees, especially in other foreign countries like Australia, Ireland, Singapore, and various Gulf countries. With the status attached to an MRCP degree, you can get better job offers, more professional benefits, and higher pay. Lastly, successfully passing the MRCP exam boosts your CV for fellowships and other medical ventures. And these benefits alone make this postgraduate degree worth it!
- Gold Standard in Medical Qualification – The MRCP exam holds prestige because of its exclusivity, making it the gold standard in types of medical qualifications. It is also mentored by the acclaimed Dr. Gurpreet Singh Wander and Dr. ArchitBoloor, both of whom have published several books and are experts in the field. Further, the MRCP exam is run by the Federation of the Medical Royal Colleges in the UK, an exclusive set of colleges that are recognised as the best in medicine. All of these factors put MRCP degree holders at the top of their field that makes it the best choice for you.
- Worldwide Symbol of Excellence – Holders of the MRCP degree can subscribe to any or all three UK Royal Colleges of Physicians, boosting their professional status and putting the MRCP exam at the top of postgraduate courses. Further, the double benefit of being able to use an MRCP degree in India and various international countries gives you wider recognition and opens more career paths in the future.
- Improves Medical Knowledge and Boosts Skill – Because of the break up into part 1 and part 2 courses of the MRCP exam, the candidate receives better medical qualifications. The paces course encourages critical thinking that mimics the qualities needed as a working doctor and thus, puts the MRCP exam at advantage over other postgraduate medical entrances. Further, to prepare extensively for the part 1 exam, Diginerveprovides a thorough course, ‘Cracking MRCP Part-1’ that consists of live webinars, video lectures, detailed course modules, and 3000 practice questions, all of which ensures improved skill and knowledge.
- Shortest Way to a Successful Medical Career – The MRCP degree is now regarded as the quickest method of reaching a successful and international medical career. The MRCP exam structure and preparation with the ‘Cracking MRCP Part-1’ course has been designed to ensure that students have the basic skills and knowledge needed in their careers. Further, being highly prepared in the first attempt ultimately leads to a shorter training time for the entire exam in comparison to other postgraduate courses.
Now that you have a basic understanding of what an MRCP degree is and how the ‘Cracking MRCP Part-1’ course can help you ace it, you can start planning for the exam. Get your MRCP books ready, find the exam date that works for you, manage the fees, and prepare to ace the MRCP exam to start your successful career as a doctor. Lastly, when you take the course with DigiNerve, you get an exclusive bank of practice questions, personal mentor support, and detailed course manuals, all of which make your preparation a smooth journey. To get started, click here.
Every medical student knows that the MRCP exam is one of the most prestigious postgraduate medical courses and allows graduates to practice medicine in India and worldwide, including Asian, European, and Gulf countries. Originally from the UK and conducted by the Royal Colleges of Physicians, the MRCP exam has two parts – part 1 and part 2 course. Part 1 is a written exam consisting of two papers, 100 best of five questions (BOF), and a time limit of 3 hours, all of which make cracking the MRCP exam very difficult. However, there are several advantages to passing the MRCP exam. Apart from being able to practice medicine in countries like Australia, Ireland, and Singapore, it also boosts your CV because of its global prestige. If you do want the wider recognition that passing the MRCP exam ensures, to get started, here are a few things to know about eligibility for an MRCP degree:
- Existing Medical Degree – The MRCP exam is for postgraduates which means that you need to obtain a bachelor’s degree before you can consider attempting it. Further, you can only apply to take the MRCP exam a minimum of one year after you have completed your medical graduation and this precious time should be spent sincerely studying for this notoriously competitive exam.
- Years of Medical Training – To apply for the MRCP exam, you need to have completed a minimum of one year of medical employment. This includes internships and other fellowships during which you have successfully gained practical medical knowledge that you will later require for the paces exam of the MRCP. To make the process easier, ensure that you have already completed your required medical employment so that you can focus on MRCP preparation.
- The Number of Attempts Allowed – The MRCP exam has a limit to the number of attempts allowed – you can attempt the MRCP medical entrance exam a maximum of six times each. Thus, you can appear for part 1 and part 2 six times each. However, you must clear part 2 and the paces course within 7 years of completing part 1. To set yourself on the right track and prevent excessive attempts, good preparation for the first attempt is the key to MRCP success. You can achieve this by rigorously using the material provided in the ‘Cracking MRCP Part-1’, a detailed MRCP preparatory course offered on DigiNerve, and guided by India’s top faculty- Dr. Gurpreet Singh Wander and Dr. Archith Boloor.
- Exam Dates and Application Process – Once you’ve studied enough and are ready to attempt the MRCP exam, you need to book an exam date. The MRCP part 1 exam dates are set three times a year, in January, May, and September, with applications opening three months before each exam date. Once you have completed your preparation with ‘Cracking MRCP Part-1’, you can apply for the exam by registering through the official Royal Colleges of the UK website.
- Fees and Age Limit – To be eligible for the MRCP exam, a fee of £594 for international applicants, and £419 for UK applicants are required. Luckily, there is no age bar imposed to appear for the MRCP exam as it is open to all students who have sufficiently prepared.
Despite being highly competitive, acing the MRCP exam is easy with expert guidance, like the acclaimed Dr. Gurpreet Singh Wander and Dr. Archith Boloor, and with a focused study plan, complete with extensive course material on an accessible platform like DigiNerve. Now that you are informed of the eligibility criteria for the MRCP exams, know that the ‘Cracking MRCP Part-1’ is the key to success. By providing students with video lectures, over 3000 BOF questions, mock tests, and mentor support, every student will have the tools needed to crack the MRCP exam. To begin your exam preparation journey, click here to get started with DigiNerve.
DigiNerve is an online medical education platform by Jaypee Brothers, and it is here to solve all the tutoring needs of medical undergraduate students, postgraduate students, and professionals. It aims to provide top-notch content to improve concept-building, acquire clinical skills, and crack exams by top-class faculty, accessible anytime, anywhere.
There are four categories of courses offered by DigiNerve: UnderGrad, PostGrad, Professional, and Exam Prep.
UnderGrad Category includes courses for 2nd, 3rd, and 4th year MBBS subjects:
- Microbiology for UnderGrads by Dr. Apurba S Sastry, Dr. Sandhya Bhat & Dr. Deepashree R
- Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait
- Pharmacology for UnderGrads by Dr. Sandeep Kaushal & Dr. Nirmal George
- Forensic Medicine and Toxicology for UnderGrads by Dr. Gautam Biswas
- Ophthalmology for UnderGrads by Dr. Parul Ichhpujani & Dr. Talvir Sidhu
- Community Medicine for UnderGrads by Dr. Bratati Banerjee
- Pediatrics for UnderGrads by Dr. Santosh T Soans & Dr. Soundarya Mahalingam
- Orthopaedics for UnderGrads by Dr. Vivek Pandey
- Medicine for UnderGrads by Dr. Archith Boloor
- Surgery for UnderGrads by Dr. Sriram Bhat M
- OBGYN for UnderGrads by Dr. K Srinivas
Additionally, two combos are also available in the UnderGrads section,
- Basic Sciences Combo: This combo includes the second professional courses (Microbiology, Pathology, and Pharmacology) along with Clinics to provide them a clinical foundation in 2nd prof.
- Clinical Combo: This combo includes Medicine, Surgery, OBGYN, Orthopaedics, Ophthalmology, Community Medicine, Pediatrics and Forensic Medicine & Toxicology course.
PostGrad Category includes PG specialisation courses:
- OBGYN MD by Dr. Aswath Kumar
- Dermatology MD by Dr. Rashmi Sarkar & Dr. S. Sacchidanand
- Ophthalmology MD by Dr. N. Venkatesh Prajna
- Pediatrics MD by Prof. Piyush Gupta
- Medicine MD by Dr. Jyotirmoy Pal and Dr. Shashank R Joshi
- Surgery MS by Prof. (Dr.) Nilay Mandal
Professional Category includes the following courses:
- Ultrasound in OBGYN Made Easy by Dr. Sonal Panchal & Dr. Chaitanya Nagori
- Basics of Infertility & IUI Made Easy by Dr. Chaitanya Nagori & Dr. Sonal Panchal
- Ganga Videos on Spine Surgery by Prof. Rajasekaran Shanmuganathan, Dr. Ajoy Prasad Shetty & Dr. Rishi Mukesh Kanna
- Advance Course in Ultrasound and Infertility by Dr. Sonal Panchal and Dr. Chaitanya Nagori
- Critical Care Simplified by Dr. Yatin Mehta, Dr. Subhal Dixit, and Dr. Kapil G. Zirpe
- Organ Donation Simplified by Dr. Kapil G. Zirpe and Dr. Rahul Pandit
- Cosmetic Botulinum Toxin Simplified by Dr. Rasya Dixit, Dr. Urmila Nischal and Dr. K.C. Nischal
Exam Prep Category includes the following courses:
- Cracking MRCOG Part 1- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 1- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 2- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 2- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 3- Live OSCEs Engagement by Dr. Richa Saxena
- Cracking MRCOG Part 3- Non-Interactive OSCEs by Dr. Richa Saxena
- Cracking MRCP Part 1 by Dr. Gurpreet Singh Wander and Dr. Archith Boloor
Why Choose DigiNerve?
The course content offered by DigiNerve is not only as per the respective curriculums but is also brought to students easily and interactively. The courses include highly illustrative video lectures, competitive self-assessment questions, progress analysis, and specially curated notes while always focusing on concept-based learning. Here are a few other aspects of DigiNerve that set it as the best guide a student can have during their Top Doc journey:
- Esteemed Faculty: Each course on DigiNerve is curated and taught by Gold Standard Faculty in the respective field. For example, ‘Cracking MRCP Part-1’ is taught by the highly acclaimed Dr. Gurpreet Singh Wander and Dr. Archith Boloor, each of whom has published research papers and taught at renowned medical universities. Similarly, ‘Ultrasound in OBGYN Made Easy’ is structured and mentored by the distinguished faculty, Dr. Sonal Panchal and Dr. Chaitanya Nagori, who have years of expertise and have published successful books on gynecology. Also, UG courses such as Microbiology for UnderGrads is taught by the maestro himself, Dr. Apurba S Sastry along with Dr. Sandhya Bhat & Dr. Deepashree R, Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait. These faculties already have an irreplaceable place on the shelves of every medical student. Thus, all students can be assured that no matter which course they choose, DigiNerve has got their back.
- Credible Content: Since all course content is structured by renowned faculty, all students get the latest medical breakthroughs, practically relevant material, clinical case demonstrations & discussions, and the benefit of over 50-year trusted medical legacy that Jaypee provides. All of this results in courses that have credible and valuable information to help students not only ace their medical and entrance exams but also develop their professional abilities as doctors.
- Easy to Use: DigiNerve is designed to be as student-friendly as possible. With an efficient and detailed website and a virtual classroom experience that is based on interactivity, all students can access courses and navigate with ease. Further, students can learn from their respective courses and content anytime and anywhere via the DigiNerve App. The app also has other great features, such as the Continue Journey Widget, Split View option to access the video lectures and notes simultaneously, Video Indexing, and ‘Ask a doubt’ feature.
- Specialization Courses: Apart from providing students with courses to help them crack competitive exams, DigiNerve also has specialized courses for doctors looking to hone in on a particular skill or for postgraduate students looking to enhance their practical knowledge. One such course is ‘Ultrasound in OBGYN Made Easy’. The course provides students with detailed knowledge of ultrasounds that is essential for gynecology and radiology practice. It also specifically teaches cutting-edge fetal medicine knowledge to help doctors reach a diagnosis.
- International Certification: On completion of the specialized courses offered in Infertility and IUI and Ultrasound in OBGYN, DigiNerve facilitates internationally recognized certificates for its students. Thus, boosting their CV, opening doors for higher pay and international practice in the respective specialization. For some courses like the USG course, students on completion receive a certificate from the prestigious Ian Donald Inter-University School.
DigiNerve is unparalleled in the quality of courses offered, the range of material taught, the Gold Standard faculty that structure and teach the courses, and the easily navigable interface. Thus, giving students helpful courses at a competitive price that provide them with conceptual clarity, allowing them to excel in their exams, and also offering practical guidance.
The MRCP Part 1 exam is your first step towards the very prestigious Royal College Membership. The exam is challenging, and students spend months preparing for it. You have to study while balancing work, recreation, and any other commitments you have going on, so it’s important to study smart. Here are some tips to prepare for the exam, so that you don’t spend crucial time trying to figure out what approach to take or what MRCP study materials to use.
Create a structured study plan
Familiarise yourself with the syllabus and estimate how much time each topic will take you depending on how fast you absorb the material. Allocate less time to topics you find easy or already know well, and more time to topics you find difficult or that require a more thorough understanding. Calculate the total time it will take you to study all of MRCP study material against the time you can spend studying in the upcoming months as well. Use your plan to stay on track with studying.
Find comprehensive course material
Online courses such as Diginerve’s Cracking MRCP Part 1 are the best comprehensive study material, as in one course, you get mentorship and webinars from distinguished faculty, a comprehensive course manual, notes, practice questions, mock exams, and performance tracking.
Do practice questions
Practice a lot. Anyone who has passed the MRCP exam will tell you that the key to passing the MRCP medical exam is to do as many MRCP practice questions as you can. Practice questions truly test your knowledge as they force you to apply what you’ve learnt. Diginerve’s Cracking MRCP Part 1 also has thousands of practice MRCP questions, ideal for thorough revision and practice.
Simulate the exam
The MRCP part 1 exam has 200 multiple choice questions split between 2 papers, each of which is 3 hours long. You need to build up stamina to keep your brain from tiring out in the middle of the medical exam. To keep working at your optimum pace throughout the MRCP medical exam, put yourself in the exact same conditions that you’ll be in when you take the exam- don’t take any breaks or talk to anyone during it. You don’t want to be sitting in the real medical exam with your brain fried and your fingers tired. The Cracking MRCP Part 1 course offers several mock exams you can take to gauge how you are doing. You can score yourself using Cracking MRCP’s mock papers, and then see how you’re doing compared to your peers on the course’s online leaderboard.
Study with a group
You may feel stressed as you study for the MRCP part 1 exam while handling work and a busy schedule. Working with others who are appearing for the medical exam will keep you motivated and make you feel like you’re not alone. When you work in groups, ideas are shared and questions are solved together. If you don’t understand a question, your friend might be able to explain it to you, which will help both your understanding and theirs.
Cracking MRCP Part 1 course offers the facility of Forums where you could interact with fellow participants and learn from each other.
The MRCP exam is one of the toughest exams to pass – but at the end of it, you walk away with an internationally recognized qualification that makes all the hard work worth it. Your job and studies are probably keeping you busy already, so it is important that you optimize your time and study for the MRCP the smart way. Here are seven tips on how to crack the MRCP Exam:
1. Stay focused on the exams
You want to allocate at least a few hours a day to MRCP exam preparation, as consistency is important. You don’t need to spend all day on the MRCP study material. Focused studying for a few hours everyday is the key to success.
2. Practice answering questions
The most important MRCP test preparation you can do is to get yourself a book of practice questions to ensure you understand the format of the test and recognize patterns in the questions. You can also try an MRCP questions bank, with Cracking MRCP Part 1, for practice.
3. Cover all the specialties in the curriculum
Try solving as many questions from the range of specialties covered in the curriculum as you can, to ensure you have a thorough knowledge of each topic. Diginerve’s app has notes and questions on every topic you need to know.
4. Find reliable MRCP study material
Make sure your MRCP study material is detailed, thorough, and covers everything you need to know. Jaypee has course manuals, revision notes, and practice papers for MRCP part 1 and MRCP part 2, and an online course with mentorship, webinars, practice questions, mock papers case studies, and revision notes for MRCP Part 1.
5. Do mock exams under timed conditions.
The MRCP tests are a marathon, not a sprint. You need to be prepared to answer hundreds of questions. Mock papers by Cracking MRCP Part 1 help you test yourself and measure your progress against peers on a leaderboard.
6. Understand the concepts, don’t just memorize
When you practice, you also need to understand the reasoning behind why an answer is wrong or right. If you only memorize, you might find yourself confused in the actual MRCP exam. Understanding the concepts will give you a better understanding and make you a better doctor overall.
7. Ask people who’ve passed the MRCP for advice
You probably know doctors who have passed the MRCP part 1 and MRCP part 2 and attained the MRCP degree. Ask them what to do and how to study. Whatever methods they used, they passed, so approaching the test in a similar way means you’re on the right track.