Becoming a specialist physician is a long, challenging but fruitful journey. Amid this journey, crossing the milestone of (Membership of the Royal Colleges of Physicians) MRCP Part 1 exam is highly crucial. To help you with details, we are here with the blog covering ‘MRCP PART 1 Exam Dates 2024.’ Here, we’ll dive deep into the specifics, studying a comprehensive guide with great insights.
What is MRCP Part 1?
The MRCP exam puts a medical student’s knowledge and skills to the test. It is a challenging exam that evaluates basic concepts not only from roots but also the practical knowledge overall. It assesses knowledge and understanding of medical sciences and the ability of a candidate to apply the knowledge in real-world situations. It is merely not an exam, it’s a pathway for the candidates who wish to specialize in medicine.
What Does MRCP Offers?
MRCP offers masters/postgraduate level medical diploma in internal medicine in the UK. It holds importance and value as it is globally recognised. It is acknowledged in the countries overall, with some being UK, UAE, Ireland, Singapore, etc. An MRCP qualified medical student/candidate can have many location options to continue medical practice. For the doctors who are preparing for specialization on the behalf of the Royal College of Physicians of Edinburgh, the Royal College of Physicians and Surgeons of Glasgow, and the Royal College of Physicians of London, the following qualifications are provided by MRCP (UK):
- MRCP (UK) Diploma
- 12 Specialty Certificate Examinations (SCEs)
What are Specialty Certificate Examinations (SCEs)?
These examinations are a chance to evaluate the candidate’s knowledge of the globally set standard. SCEs cover all that’s required to know, by a newly qualified specialist in the chosen field. These are required for specialist physicians in the UK.
What is the Difference Between MRCP Part 1 and Part 2?
Understand it as ‘MRCP Part 1 being the foundation where basic medical and clinical knowledge is tested’ and ‘MRCP Part 2′ being the practical application of what the medical professional has learnt!’
| MRCP Part 1 | MRCP Part 2 |
| Foundation of Basic Medical Knowledge | Practical Application of What’s Leant |
| MCQ Style Questions | Image Based Questions & Clinical/Medical Scenarios |
| Tests Common Disorders & Clinical Sciences | Evaluates Decision Making/Reactions Under Pressure |
What are MRCP Part 1 Dates 2024?
Mark your calendars! Here are the crucial upcoming dates for the MRCP Part 1 exam in 2024:
- 14 August 2024: Application period from 3 June to 10 June 2024.
- Results by 13 September 2024.
- 16 October 2024: Application period from 5 August to 12 August 2024.
- Results by 15 November 2024.
- 22 January 2025: Application period from 4 November to 11 November 2024.
- Results by 21 February 2025.
- 16 April 2025: Application period from 3 February to 10 February 2025.
- Results by 16 May 2025.
This calendar is a reminder of stepping closer to your goal. So, plan and prepare for MRCP beforehand to be all set when the time comes.
What is MRCP PART 1 Exam Syllabus and Format?
The MRCP Part 1 exam is composed of two papers, each with 100 MCQs. Total time is three hours to complete the exam. Here’s a snapshot of what you need to cover for the exam. Don’t forget to revise all of it.
How to prepare MRCP PART 1? (Key Concepts)
Here’s the snapshot of what needs to be grasped!!!
- Cardiology: Heart diseases, ECG interpretation
- Respiratory Medicine: Asthma, COPD
- Gastroenterology: Liver diseases, inflammatory bowel disease
- Neurology: Stroke, epilepsy
- Endocrinology: Diabetes, thyroid disorders
- Rheumatology: Arthritis, connective tissue diseases
- Nephrology: Acute kidney injury, chronic kidney disease
- Infectious Diseases: HIV, tropical diseases
- Hematology: Anemias, clotting disorders
- Oncology: Cancer types, treatments
- Psychiatry: Mood disorders, schizophrenia
- Ophthalmology: Eye diseases, vision tests
- Dermatology: Skin infections, dermatologic conditions
- Clinical Pharmacology: Drug mechanisms, side effects
How to Prepare MRCP Part 1? (Tips & Tricks)
Preparation is the key to success! For cracking MRCP Part 1, a smart/strategic vision can make all the difference. Here are some tips to get you started:
- Always Make a Plan: Note down topics and make a well-structured study plan.
- Use Quality Resources: Enroll for digital courses and classes, and start a guided journey. One such being ‘Cracking MRCP Part 1’ by Dr Gurpreet Singh Wander and Dr Archith Boloor.
- Practice Makes a Man Perfect: Practice the MCQs, solve question banks, and research online. A good digital course will always provide you practice exercises too.
- Join Study Groups: A collective learning can assist you get different perspectives and clarify doubts. Join online forums or local study groups to discuss tricky topics.
- Keep a Note of UK Medicine Area: Indian students need to have an edge over this! A candidate must have knowledge of UK internal medicine training, UK’s guidelines, and other important breakthroughs in UK medical science.
It is a difficult exam but only for those who do not prepare! Just be on time. From online application dates to having a note of closing deadline, from initial preparation of sample questions to final exam preparation, leave no chance for delays. Also, stay stress-free, especially on the exam day to have 100% chance of success. Stress is the biggest enemy. So, to win over a wide range of subjects from the syllabus, just be confident and stress-free.
What is the MRCP Part 1 Fees in India?
While enrolling, the Indian students registering from India need to pay around £616 as fee for the MRCP Part 1 exam as they are international students. For the UK, the application procedures include fee as £460. The fees may vary, so it’s best to check the MRCP UK website for the latest information.
To be eligible for the MRCP Part 1 exam, a candidate must:
- Hold a medical degree recognized by the General Medical Council (GMC) or equivalent.
- Have completed at least one year of postgraduate medical experience.
Understanding MRCP Part 1 Results
The MRCP Part 1 results are usually released 4 to 6 weeks after the exam. The results are published online on the MRCP UK website, where you can log in to view your scores. The pass mark usually hovers around 540, but it’s adjusted based on the exam’s difficulty through a process called equating.
Final Thoughts
The MRCP Part 1 exam is a crucial milestone in a medical career. With a detailed understanding of the schedule, key dates and prep strategies, this exam can be cracked! With the right resources, regular practice, and staying up to date with official updates and news, a candidate can pass this exam with flying colors. Let’s remember, the MRCP Part 1 is not just an exam; it’s a steppingstone to a fulfilling career in medicine. Your journey to becoming a specialist physician begins here!
Note: For more detailed information and to stay updated with the latest announcements, visit the MRCP UK website.
Frequently Asked Questions (FAQs)
Q1. What is the MRCP Exam 1 Format?
Ans. Exam Format is as follows:
- The MRCP Part 1 exam consists of two 3-hour papers.
- It is in the MCQ (Multiple-Choice-Questions) format.
Q2. What is the MRCP Part 2 Exam Format?
Ans. The MRCP Part 2 is further in two parts. One is Written and the other is Clinical Examination, known as PACES.
- The ‘Written’ consists of a three-hour MCQ based question paper including diagnosis, investigations & prognosis of patients.
- The ‘PACES’ includes 5 clinical stations series, each evaluated by two examiners.
Q3. When can we Register for the Upcoming MRCP Part 1 Exam?
Ans. At present, application process can start from 5th August to 12th August 2024. It is for the exam to be held on 16th October, 2024. The results could be out by 15th November, 2024. The rest of examination dates have been mentioned above in the blog, in detail.
Q4. What is the fee for MRCP Part 1 Exam?
Ans. The fee is around £460 for (UK) and £616 for international students. However, there could be slight changes in the fee depending upon various factors. It is always advisable to reach out to the official website of MRCP for the exact fee structure.
Everything is made for a defined purpose anything which is not intended for further use is termed waste. In the scientific and industrial eras combined with the increasing population, the turnover of products has gone very high increasing the quantum of urban solid waste. With the increased need for health care in a changing society the role of hospitals/nursing homes comes to the forefront.
Hospital waste or types of healthcare waste should include any material generated in healthcare establishments including aqueous and other liquid waste.
Hospital waste means any solid, fluid, or liquid waste material including its container and any other intermediate product which is generated during short-term and long-term care consisting of observational, diagnostic, therapeutic, and rehabilitative services for a person suffering or suspected to be suffering from disease or injury and for parturient or during research of production and testing of biological during immunization of human being.
Types of Healthcare waste facilities are responsible for managing healthcare waste generated within their facilities, as well as waste generated through activities in the community. These facilities must undertake proper segregation, collection, in-house transportation, pre-treatment, and waste storage before handing it over to a Common Bio-medical Waste Treatment Facility (CBWTF) operator.
Therefore, proper management of healthcare waste at these facilities necessitates that all categories of staff understand and adhere to the technical requirements for waste handling as per the Biomedical Waste Management Rules, 2016.
Classifications of Waste Generated from Healthcare Sectors
1. Bio-Medical Waste
It refers to any waste produced during diagnosis, treatment, or immunization of humans or animals as well as related research activities, or during the production or testing of biologicals in health camps. This includes all waste from healthcare facilities that could potentially harm human health or the environment if improperly disposed of. Such waste is considered infectious and must be managed according to the Biomedical Waste Management Rules of 2016 to prevent adverse effects on health or the environment.
Around 10% to 15% of the total waste generated by healthcare facilities constitutes biomedical waste. This category includes materials that have come into contact with patients’ blood, secretions, infected body parts, biological fluids, chemicals, medical equipment, pharmaceutical waste, laboratory discharge, sharp objects like needles and glassware, and plastics.
According to the Biomedical Waste Management Rules of 2016, this waste is categorized into four types based on how it is segregated and color-coded. Each category includes specific types of biomedical waste, as given below:
- Yellow Category
- Red Category
- White Category
- Blue Category
These categories are divided as per the types of waste under each category as follows:
| Category | Type of Waste |
| Yellow | Human Anatomical Waste
Human tissues, organs, body parts, and fetus below the viability period (as per the Medical Termination of Pregnancy Act 1971, amended from time to time). |
| Animal Anatomical Waste
Experimental animal carcasses, body parts, organs, and tissues, including the waste generated from animals used in experiments or testing in veterinary hospitals or colleges, or animal houses. |
|
| Solid Waste
Items contaminated with blood, body fluids like dressings, plaster casts, cotton swabs, and bags containing residual or discarded blood and blood components. |
|
| Discarded Medicine
Pharmaceutical waste like antibiotics, and cytotoxic drugs including all items contaminated with cytotoxic drugs along with glass or plastic ampoules, and vials. Etc. |
|
| Chemical Waste
Chemicals used in the production of biological and used or discarded disinfectants. |
|
| Chemical Liquid Waste
Liquid waste is generated due to the use of chemicals in the production of biological and used or discarded disinfectants, Silver X-ray film developing liquid, discarded Formalin, infected secretions, aspired body fluids, liquid from laboratories, and floor washings, cleaning, housekeeping and disinfecting activities, etc. |
|
| Discarded linen, mattresses, beddings contaminated with blood or body fluid, routine mask & gown. | |
| Microbiology, Biotechnology, and other clinical laboratory waste (Pre-treated) | |
| Microbiology, Biotechnology, and other clinical laboratory waste: Blood bags, laboratory cultures, stocks or specimens of microorganisms, live or attenuated vaccines, human and animal cell cultures used in research, industrial laboratories, production of biological, residual toxins, dishes, and devices used for cultures. | |
| Red | Wastes are generated from disposable items such as tubing, bottles, intravenous tubes and sets, catheters, urine bags, syringes without needles, fixed needle syringes with their needles cut, vacutainers, and gloves. |
| White | Waste Sharps Including Metals
Needles, syringes with fixed needles, needles from needle tip cutters or burners, scalpels, blades, or any other contaminated sharp object that may cause punctures and cuts. This includes both used, discarded, and contaminated metal sharps. |
| Blue | Broken or discarded and contaminated glass including medicine vials and ampoules except those contaminated with cytotoxic wastes. |
2. General Waste
General waste includes all waste other than biomedical waste that has not been in contact with hazardous waste or infectious materials, chemicals, or biological secretions, and does not include sharp objects. This type of waste typically includes:
- Newspaper, paper, and cardboard boxes
- Plastic water bottles
- Aluminum cans from soft drinks
- Packaging materials
- Food containers after removing leftover food
- Organic or biodegradable waste, mainly food waste
- Construction and demolition waste
These general wastes are classified as wet wastes and dry wastes and should be collected separately. The quantity of general waste is around 85% to 90% of the total generated from the facility.
3. Other Wastes
Other wastes include electronic devices such as batteries and radioactive materials that are not classified as biomedical waste. They must be disposed of according to specific regulations: the E-waste (Management) Rules of 2016, the Batteries ( Management & Handling) Rules of 2001, and the rules or guidelines established under the Atomic Energy Act of 1962, depending on the type of waste generated.
Guidelines for Management of Healthcare Waste Categories as per Biomedical Waste Management Rules, 2016
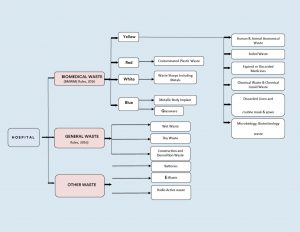
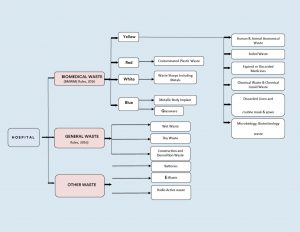
Figure 1: Categorization & Classifications of Wastes in Health Care Facilities.
Color Coding and 4 types of dustbins in hospitals used for Waste Segregation & Collection
According to Schedule I of the Bio-Medical Waste Management Rules of 2016, healthcare facilities (HCFs) must use specific color-coded dustbins and types of containers/bags for segregating and collecting biomedical waste generated within the facility.
| Category | Type of Waste | Colored Container & Type of Container | Treatment Options as per Schedule I |
| Yellow Category |
|
Yellow-colored non-chlorinated Plastic Bags.
NOTE: |
Incineration/deep burial |
| Red Category |
|
Red Colored Non-Chlorinated Plastic Bags (having thickness equal to more than 50u) and containers. | Autoclaving/microwaving/chemical treatment |
| White Category |
|
White Colored translucent puncture-proof, leak-proof, tamper-proof containers. | Autoclaving/microwaving/chemical treatment and destruction/shredding |
| Blue Category |
|
Puncture-proof, leak-proof boxes or containers with blue-colored markings. | Disposal of wastes and secured landfill |
Bio-Medical Waste Collection
Time of Collection
- Daily Collection: Ensure daily collection from each hospital ward at fixed intervals.
- Timing Adjustments: Schedule collections based on waste generation patterns throughout the day.
- Separate Collection: Avoid collecting general waste concurrently with biomedical waste.
- Visitor Waste Management: Collect general waste immediately after visiting hours to prevent accumulation.
- Personal Protective Equipment: Provide PPE to staff handling biomedical waste.
Packaging
- Filling and Sealing: Fill biomedical waste bags and sharp containers up to three-quarters full and seal them promptly.
- Sealing Methods: Use ties or plastic tags to seal bags to avoid stapling.
- Availability of Replacement: Ensure replacement bags or containers are readily available at collection points.
- Labeling Requirements: Label bags and containers with biohazard symbols, including details like date, type of waste, quantity, and sender’s and receiver’s information.
- Barcode Compliance: Affix barcoded labels on the bag as per CPCB guidelines.
Labeling
- Biohazard Symbols: Clearly label all bags, containers, and bins with biohazard or cytotoxic symbols as per BMWM Rules, 2016.




Interim Storage
- Minimization: Discourage interim storage of biomedical waste in patient care areas.
- Designated Areas: Store biomedical waste temporarily in designated, low-traffic areas if necessary.
Treatment Option for Bio-medical Waste Types
| Treatment Options | Biomedical Chemical Processes |
| Thermal Processes Low-heat Systems (93-177oC) |
|
| High-heat Systems |
|
| Mechanical Processes |
|
| Irradiation Processes |
|
| Biological Processes |
|
| Considerations for Processing Incineration |
|
| Autoclaving |
|
| Microwaving |
|
| Deep Burial |
|
| Sharp Materials Disposal |
|
| Radioactive Waste |
|
| Mercury Control |
|
Frequently Asked Questions (FAQs)
Q1. What is clinical waste, and how is it different from infectious waste?
Ans. Clinical waste includes all waste generated from medical facilities, including non-infectious materials like packaging and expired medications, whereas infectious waste refers to waste contaminated with pathogens, such as bacteria, viruses, or other microorganisms.
Q2. What are the proper disposal techniques for biomedical waste, particularly sharps waste?
Ans. Sharp waste like needles and scalpels, must be disposed of in puncture-proof containers specifically designed for sharps disposal. These types of containers are sealed and handled carefully to prevent injuries and potential infections during disposal.
Q3. How does improper medical waste management contribute to the spread of diseases?
Ans. Improper management of biohazardous waste can lead to contamination of the environment and increase the risk of spreading infectious diseases. Pathogens present in medical waste, if not managed correctly, can infect healthcare workers, patients, and the normal public.
Q4. What is some risk associated with inadequate handling of pathological waste?
Ans. Pathological waste which includes tissues, organs, and body parts, poses significant health risks if not properly managed. Exposure to such waste can lead to infections or exposure to hazardous chemicals used in treatments.
Q5. Why is it important for medical facilities to use appropriate medical waste containers?
Ans. Medical waste containers are designed to safely store and transport various types of medical waste, including biohazardous materials and sharps. Using proper containers minimizes the risk of accidental exposure and ensures compliance with regulations for safe disposal.
DigiNerve is constantly evolving to enhance your experience while you’re on your journey to becoming a Top Doc. We are excited to bring you the latest updates with our commitment to ensure a seamless journey on the go.
Read on the July edition (Vol – 1) of our monthly newsletter to know the latest updates.
CONTENT UPDATES
PostGrad Course Updates
Dermatology MD:-
1. Chat show on ‘Discussion on Leprosy’ by Dr. Vivek Vasudev Pai, Dr. Shraddha Mahobia, and Dr. Samira Siddiqui Khatoon Mohd. Hanif has been added to the course.
Learning Outcomes of the chat show were:
- To learn the approach to a patient with leprosy.
- To understand the current scenario of leprosy and the National Strategic Plan for 2023-2027 for India.
- To learn the approach to patients with lepra reactions and relapse.
- To understand the management of patients with ENL reactions and relapse.
Pediatrics MD:-
1. Chat show on ‘Approach to a Child with Asthma’ by Dr. Piyush Gupta and Dr. Prawin Kumar has been added to the course.
Learning Outcomes of the chat show were:
- Clinical presentation of asthma in children.
- How can a diagnosis of asthma in children be established?
- What is the role of the Pulmonary Function Test (PFT) in the diagnosis of asthma.
- Management of Asthma in Children.
Medicine MD:-
1. 8 new topics have been added to the following modules:
| Module | Section | Topic |
| Rheumatology | Long Case Discussions | Gout |
| Infectious Diseases | Clinical Scenarios | Amoebic Liver Abscess |
| Systemic Fungal Infections | ||
| Japanese Encephalitis | ||
| Critical Care Medicine | Decision Making | Central Venous Line |
| Intubation in Critically Ill Patients | ||
| Cardiology | Basic Sciences | Treadmill Test |
| Endocrinology and Diabetes | Long Case Discussions | Approach and Management of Hyponatremia |
Note: The topics mentioned above also include 39 new self-assessment and 16 benchmark trials.
Update Your DigiNerve App for Better Experience.
To read the updates shared in the Monthly Newsletter June (Vol-2), click here.
DigiNerve is constantly evolving to enhance the user experience while you’re on their journey to becoming a Top Doc. We are excited to bring the latest updates with our commitment to ensure a seamless journey on the go.
Read our monthly newsletter’s June edition (Vol – 2) for the latest updates.
CONTENT UPDATES
PostGrad Course Updates
OBGYN MD:-
1. 5 new topics have been added to the following modules:
| Section | Module | Topic |
| Gynecology | Menstrual Abnormalities | Menopause Hormonal Therapy |
| Obstetrics | Procedural Videos | Caesarean Section |
| Third Stage of Labour and its Complications | Postpartum Psychiatric Illness | |
| Medical Disorders in Pregnancy | Case Discussion: Pregnancy Induced Hypertension | |
| Labour (Normal and Abnormal) | Management of Abnormal Labour |
Note: The topics mentioned above also include 25 new MCQs and 10 benchmark trials.
2. Chat show on ‘Primary Amenorrhea’ by Dr. Aswath Kumar and Dr. Lilly Varghese has been added to the course:
Learning Outcomes of the chat show were:
- Different etiologies of primary amenorrhea
- Important subtypes: Clinical features
- Investigations
- Management: Hormonal and surgical treatment
Surgery MS:-
1. Chat show on ‘Management of Head Injury’ by Prof. (Dr.) Nilay Mandal and Dr. Arjun Dasgupta has been added to the course.
Learning Outcomes of the chat show were:
- Initial assessment of a head injury patient
- Prevention of secondary injury and management of raised ICP
- Types of head injury and their radiological findings
Professional Course Updates
MRCOG Part 2:-
1. Webinar on ‘Discussion of Important Questions and Doubt Clearance (MRCOG-2 EMQs)’ by Dr. Richa Saxena has been added to the course.
Learning Outcomes of the webinar were:
- To discuss important questions of MRCOG part 2 exam.
- To prepare for exam with the help of carefully curated questions with detailed explanations, images and flowcharts.
- To ease the journey of clearing MRCOG exam.
- To understand latest patterns of questions as per RCOG curriculum (EMQs).
Technology Updates
1. Inclusion of HYQs
A new section of High Yield Questions has been included in the courses- Cracking MRCOG- PART 1 and Part 2. It comprises HYQs from the year 2016-2022.
2. Free Access to Dr. Wise
An additional benefit of 10 queries for non-subscribers.
3. Customised Question Bank Generator
- A new feature of Customised Question Bank Generator has been added, under the course of Cracking MRCOG Part-1.
- Beneath the ‘Test’ section, users can generate questions in the ‘Practice’ or ‘Test Mode’ as per the choice of difficulty level and as per the number of questions required.
Update Your DigiNerve App for Better Experience.
To read the updates shared in the Monthly Newsletter July (Vol-1), click here.
Overview
Ventilation is an important area of respiratory care and aims to ensure the proper gas exchange within the lungs.
The respiratory and cardiovascular systems collaborate to supply oxygen O2 to tissues and release carbon dioxide, CO2.
When patients experience respiratory difficulties, there is often an elevation in CO2 levels in their blood gases.
Strategies to address this include airway clearance through suction and mechanically augmented respiratory parameters such as atmospheric pressure rate, respiratory rate, pressure, or volume to enhance ventilation.
To achieve the required pressure for mechanical ventilation, access to the airway is imperative. This access is typically facilitated through methods such as:
- Oral or nasal endotracheal tube (ETT)
- Tracheostomy Tube
- Well-sealed mask for non-invasive ventilation
These methods ensure efficient delivery of ventilatory support, thereby aiding in maintaining adequate gas exchange in the lungs.
There are two primary common modes of ventilation:
- Invasive Ventilation: Utilized for unconsciousness patients.
- Non-invasive Ventilation: Suitable for conscious patients.
These various techniques of mechanical ventilation are important topics for exams like NEET-PG/next and FMGE.
What are the different types of ventilator modes?
Different methods/modes of ventilation, offers tailored treatment plan that respond to the patient’s specific pathology and requirements.
| Controlled Modes | Supported Modes | Combined Modes | Spontaneous Breathing |
| Volume Control | Pressure Support | AUTOMODE: Volume Control- Volume Support | Continuous Positive Airway Pressure |
| Pressure Control | Volume Support | AUTOMODE: Pressure Control – Pressure Support | Nasal Continuous Positive Airway Pressure |
| Pressure-Regulated Volume Control | Non-Invasive Ventilation- Pressure Support | AUTOMODE: Pressure-Regulated Volume Control – Volume Support | |
| Non-Invasive Ventilation – Pressure Control | Synchronized Intermittent Mandatory Ventilation: Volume Control+ Pressure Support | ||
| Synchronized Intermittent Mandatory Ventilation: Pressure Control+ Pressure Support | |||
| SIMV: Pressure-Regulated Volume Control+ Pressure Support |
There are different types of Ventilator modes which are divided up into pressure or volume-controlled modes, this modern approach classifies ventilatory modes based on three characteristics: the triggers (Flow versus pressure), the limit (what determines the size of the breath), and the cycle (What ends the breath).
1. Controlled Mandatory Ventilation (CMV)
Also known as Assist-Control Ventilation, is a mode of mechanical ventilation where each mandatory breath is either as assist or control breath, all delivered with the same preset volume or partial pressure.
This mode is particularly suitable for patients who require minimal breathing effort, as the ventilator fully controls the patient’s total breathing. CMV is indicated in patients with severe neurological alterations, deep sedation, shock, or respiratory failure. CMV is a common way to decrease the intracranial pressure after head injury.
It ensures consistent ventilation regardless of the patient’s inspiratory efforts. It’s crucial to note that CMV does not eliminate work of breathing entirely, as the diaphragm may still be active.
Therefore, patients should be heavily sedated, and drugs like fentanyl, dexmedetomidine, or midazolam can be used to achieve this level of sedation.
Features of Controlled Mandatory Ventilation:
- Physical Character: Pressure is being controlled.
- Tidal Volume: Tidal Volume is around 7-8ml/Kg.
- Patient Efforts: No efforts from the patient’s side.
- Usage: Typically used in heavily sedated patients.
- Effect on BP and Urine Output: May lead to decrease in BP and urine output due to controlled ventilation.
2. Assist-Control Ventilation
It is a mode of mechanical ventilation where each mandatory breath is either an assist or control breath, all delivered with the same preset volume or partial pressure.
This mode is particularly suitable for patients who require minimal breathing effort, as the ventilator fully controls the patient’s total breathing. CMV is indicated in patients with severe neurological alterations, deep sedation, shock, or respiratory failure. CMV is a common way to decrease intracranial pressure after a head injury.
It ensures consistent ventilation regardless of the patient’s inspiratory efforts. It’s crucial to note that CMV does not eliminate the work of breathing, as the diaphragm may still be active.
Therefore, patients should be heavily sedated, and drugs like fentanyl, dexmedetomidine, or midazolam can be used to achieve this level of sedation.
Features of Controlled Mandatory Ventilation:
- Physical Character: Pressure is being controlled.
- Tidal Volume: Tidal Volume is around 7-8ml/Kg.
- Patient Efforts: No efforts from the patient’s side.
- Usage: Typically used in heavily sedated patients.
- Effect on BP and Urine Output: This may lead to a decrease in BP and urine output due to controlled ventilation.
3. Synchronized Intermittent Mandatory Ventilation (SIMV)
SIMV is a ventilator mode that offers partial mechanical assistance while allowing the patient to breathe spontaneously.
Unlike Assis-control ventilation, in SIMV, the patient’s breaths are partially on their own, reducing the risk of hyperinflation or alkalosis. Mandatory breaths are synchronized with spontaneous respirations, providing support when needed.
SIMV may increase the work of breathing and reduce cardiac output, potentially prolonging ventilator dependency. The addition of pressure support to spontaneous breaths can alleviate some of the work of breathing.
SIMV is often used as a weaning mode, allowing patients to gradually regain their respiratory function. Moderate sedation is typically required to ensure patient comfort and synchronization with the ventilator.
SIMV is indicated for conditions such as high risk of hyperventilation/respiratory alkalosis due to increased respiratory rate, pulmonary edema, acute respiratory distress syndrome, neuromuscular disorders, and cardiac thoracic surgery. It’s typically avoided in patients with shock and head injuries.
Features of Controlled Synchronized Intermittent Mandatory Ventilation:
- Physical Character: Respiratory rate (RR) is 14/min.
- Tidal Volume: Tidal Volume is 400ml/Kg.
- Patient Efforts: Allows for some spontaneous sedation.
- Usage: Can be used in patients with no or slight sedation.
- Effect on BP and Urine Output: May have less impact on BP and urine output due to less protective ventilation compared to CMV.
4. Pressure Control Ventilation
It is a common ventilator mode that offers less risk of barotrauma compared to assist control ventilation and SIMV, as it does not allow for patient-initiated breaths. In PCV, the respiratory flow pattern decreases exponentially, reducing peak pressures and improving gas exchange.
However, there are no guarantees for volume especially when lung mechanics are changing, making it traditionally preferred for patients with neuromuscular disease but otherwise normal lungs.
Pressure is fixed manually, and the ventilator decides the volume. PCV is mainly used for conditions like Acute Respiratory Distress Syndrome (ARDS). A major drawback of this mode is the risk of endotracheal tube obstruction due to secretions, leading to reduced volume reaching the patient’s lungs and resulting in respiratory acidosis due to poor oxygenation and increased CO2 levels.
Features of Pressure Control Ventilation:
- Physical Character: Operates on pressure control, maintaining set inspiratory pressure.
- Tidal Volume: Not designed specifically as a weaning mode.
- Patient Efforts: Facilitates spontaneous breathing efforts.
- Usage: Commonly employed in pediatric patients due to its adaptability.
- Effect on BP and Urine Output: May exert less influence on blood pressure and urine output as it allows for spontaneous breathing, potentially improving oxygenation without significantly impacting cardiovascular function.
5. Pressure Support Ventilation
PSV is a spontaneous mode of ventilation where each breath is initiated by the patient but supported by constant pressure inflation.
It operates two mechanisms: CPAP (Continuous Positive Airway Pressure) and PEEP (Positive End-Expiratory Pressure), which helps open the alveoli. PSV allows the patient to determine inflation volume and respiratory rate, although pressure remains controlled by the ventilator.
Therefore, it can only augment spontaneous breathing, typically with pressures ranging from 5-10cm H2O, especially during weaning. PSV can be delivered through specialized face masks.
Features or Pressure Support Ventilation:
- Physical Character: Works on pressure control
- Tidal Volume: Not a weaning mode.
- Patient Efforts: Facilitates spontaneous breathing.
- Usage: Often used in pediatric patients.
- Effect on BP and Urine Output: This may have less impact on BP and urine output, as it allows for spontaneous breathing and may improve oxygenation.
6. Volume Control Ventilation
In the mode of ventilation, the ventilator delivers a predetermined tidal volume to the patient with each mandatory breath. This mode is typically synchronized with the patient’s inspiratory effort, ensuring that the desired tidal volume is consistently delivered. Volume control ventilation is commonly used in patients with normal lung compliance and resistance, as it helps maintain a consistent ventilation pattern.
Another mode of volume ventilation is Assist-Control Ventilation (ACV). ACV combines the features of volume control ventilation with the ability to support spontaneous breathing efforts. In this mode, the ventilator delivers a set tidal volume with each breath initiated by the patient.
Features of Volume Control Ventilation:
- Physical Character: Operates on volume control, delivering a predetermined tidal volume.
- Tidal Volume: Delivers a set tidal volume.
- Patient Efforts: Patient effort can initiate the breath, but the ventilator ensures that the desired tidal volume is delivered.
- Usage: Commonly used in patients with normal lung compliance and resistance.
- Effect on BP and Urine Output: Volume control ventilation may increase intrathoracic pressure, which can have an effect on blood pressure and urine output. However, the impact can vary depending on the patient’s condition.
7. PEEP (Positive End-Expiratory Pressure)
PEEP level helps to keep the alveoli open at the end of expiration and helps in increasing partial pressure, thereby aiding in improving patient oxygenation. This increase in intrathoracic pressure typically leads to a reduction in venous pressure and carbon dioxide levels. However, it is essential to note that while a decrease in blood pressure might occur, it doesn’t necessarily always result in decreased urine output. Positive End-Expiratory Pressure, expressed in centimeters of water (cmH2O), applies pressure at the end of exhalation, thereby preventing the air sacs in the lungs from collapsing and further improving oxygenation.
8. CPAP (Continuous Positive Airway Pressure)
It is commonly employed to assess a patient’s readiness for extubating, particularly when minimal ventilation support is required.
It maintains a constant circuit pressure as specified by the operator throughout ventilation. Pressure Support Ventilation is often combined with CPAP, providing positive pressure assistance throughout the breathing cycle.
PSV can be delivered through a mask and is utilized in conditions such as obstructive sleep apnea, especially when utilizing a nasal mask.
Additionally, it can be used to delay intubation or manage acute exacerbations of Chronic Obstructive Pulmonary Disease, respiratory distress syndrome, or acute lung injury.
9. Airway Pressure Release Ventilation
It delivers a constant high artificial airway pressure to ensure oxygenation, while ventilation occurs through the release of that pressure.
During the majority of the cycle, a continuous high pressure is applied for a set duration followed by a brief period of lower pressure. The concept revolves around maintaining constant alveolar volume during the extended T high phase (covering 80%-90% of the cycle), enhancing oxygenation.
This extended period of high pressure, often termed an open lung strategy minimizes the repetitive inflation and deflation of the lungs observed in other ventilation modes, thus mitigating the risk of ventilator-induced lung injuries.
APRV offers a unique approach to optimizing respiratory mechanics in critically ill patients in the intensive care unit, reducing the respiratory effort required for ventilation.
Frequently Asked Questions (FAQs)
Q1. What are potential complications associated with the intermittent Mandatory Ventilation mode?
Ans. One notable complication of IMV is breath stacking, characterized by a spontaneous breath occurring immediately after a mechanical breath. This sequence can elevate Peak Inspiratory Pressure (PIP), posing a risk of barotrauma and cardiac compromise.
Q2. How do ventilators work in the Intensive Care Unit ICU?
Ans. In the ICU, mechanical ventilators, provide positive pressure ventilation, adjusting ventilator settings like inspiratory time and respiratory cycles to optimize oxygenation. They support patients with respiratory failure while considering factors such as venous return and the effects of positioning, like the prone position, to improve the ventilation-perfusion ratio.
Q3. What happens when the ventilator pressure goes to zero during mechanical ventilation?
Ans. When the ventilator pressure drops to zero, the elastic recoil of the lungs pushes air out. However, the time allotted for exhalation may not be sufficient for all the air to leave the lungs completely.
Q4. What are the advantages of Pressure Control Ventilation?
Ans. Pressure control ventilation offers several advantages, it allows for precise control of alveolar pressure, promoting lung protective ventilation strategies. This ventilatory mode enables adjustment of inspiratory flow rates and initial ventilator settings tailored to individual needs. Respiratory therapists can optimize therapy by titrating the pressure support level, ensuring a favourable pressure gradient for adequate gas exchange.
The transplant coordinator in organ donation plays a crucial role in patient care during the entirety of the transplant process including pre-transplant evaluation, waitlist management, transplant admission, and discharge/post-transplant follow-up.
These crucial functions are dependent upon the organization, critical thinking capabilities, recent research, and the adept utilization of evidence-based practices. The role of transplant coordinator demands exceptional interpersonal skills to effectively collaborate with patients, their families, support systems, members of the transplant team, and referring providers.
There are two types of transplant coordinators: procurement coordinators and clinical transplant coordinators. Both clinical and procurement coordinators are actively involved in planning, evaluating, and maintaining records, but the most important part of their job is supporting individuals and families.
Let’s embark on a journey to learn about organ donation and the role of the transplant coordinator, from the initial process of evaluation to the delicate post-transplant care or surgery.
What is an Organ Donation?
Organ donation is a surgical process in which a failing organ is replaced with a healthy one from a donor who no longer needs it. Typically, organ donors are people who have recently volunteered before their declaration of death to donate organs afterward, or their family or close relatives decide on their behalf. This process is human compassion and has a crucial impact on patient care and survival. For those people/patients who are suffering from organ failure have a second chance at life, from organ donors as a selfless act. Behind this process, there’s a well-coordinated complex network between the transplant team to ensure the ethical and safe transfer of organs from donor to recipient.
The receiver will be a patient who is suffering from organ failure and will not be able to live without an organ transplant, this organ recovery process is referred to as retrieval.
Health care providers must collaborate with the medical team to recover, and preserve, organs and tissue donation from both living donors or after the donor’s death. Health care provider needs to educate the concerned families about myths and concerns surrounding the organ donation process which can help increase the number of donor organs due to which fewer patients will die from a lack of organ or tissue donor.
What is the Process for Organ Donation?
It is an act of selflessness, offering a new gift of life for patients battling with organ failure. It starts with the decision made by their family and donor to donate organs. This process includes the most important aspect which is the consent of the organ donor for transplant coordinator.
This complex process includes a professional or dedicated team of experts or healthcare professionals working to ensure the ethical transfer of organs from organ donors to compatible organ recipients. The transplant coordinator explains the whole process and benefits of organ donation to the families and ensures all legal formalities are done once the decision is made, after the transplant coordinator steps in to facilitate the organ transfer process.
Transplant coordinators play a crucial role in coordinating with various stakeholders, and medical professionals, including the donor’s family, transplant centers, and potential recipient. The process of organ donation is regulated in India by the Transplantation of Human Organs & Tissues Act which is divided into two categories.
1.Organ donation in India after death (Brain death organ donation)
For deceased donors, the process of organ donation starts with evaluating the donor’s condition to make it a favorable environment for organ donation which includes factors i.e. stabilizing the arterial blood pressure, and cardiac output by providing ventilatory support.
When the donor’s death is confirmed using either circulatory or neurological criteria, the family is approached after the following confirmation to obtain legal consent to discontinue life support from the patient. This process of organ and tissue procurement procedures is done carefully because inflammatory mediators enter the solid organs after death, which increases the organs’ immunogenicity.
When a potential donor is near death or has already passed away then the organ procurement coordinator is informed by notification which contains detailed information about patient-related data i.e. medical history, age, cause or expected cause of death, family contact information, and other relevant data.
The organ procurement organization responsibilities during the process proceed to:
- Schedule additional examinations if deemed necessary.
- Check for prior consent for the donation process from the patient or presence in the state or central donor registries. If the patient is unavailable, seek authorization from their blood relatives, like spouses, children, parents, or legal guardians.
- Ensure the patient remains on artificial life support until authorization is obtained.
- Connect with the state organ transplant center to initiate a search for matching recipients.
- Receive recipient evaluation list generated by the state organ transplant center based on factors like tissue type, height, blood sample for blood type, weight, distance, waiting time, and disease severity.
- Contact potential recipients based on the provided list.
- The transplant surgeon makes the final decision based on the recipient’s health, organ suitability, and availability of local recipients.
- Coordinate consent process and organ matching for the receiving (recipients).
- Transport the donor’s body to the mortuary, placing saline-soaked gauze over the eyes until harvesting is complete.
- Conduct organ removal by surgeons following standard surgical procedures which include incisions in a sterile operative platform.
- Preferentially procure heart and lungs followed by liver, pancreas, and kidneys.
- Store procured organs in a cooling environment at 4 degrees Celsius to mitigate damage from blood flow restriction, although this doesn’t halt all cellular processes.
- Store immediately removed organs in a sterile container filled with icy slush to prevent freezing during transport.
- Surgically close open incisions.
- Arrange rapid transport to the receipt center as organs and tissues lose viability quickly.
2.The living organ donation process includes two main categories for living organ donors:
- Non-relatives and close relatives:
- The candidates for donation are typically genetically related to the recipient and are above 18 years old. Examples include sons, daughters, parents, siblings, grandparents, or grandchildren.
- Organs can be procured after their clinical brain death diagnosis or with approval from the authorization committee.
- Unrelated Donors for Social Welfare:
- These donors donate for social welfare purposes and may not have a genetic relationship with the recipient in which the social worker plays a crucial role in this process.
- Organ procurement can occur after their clinical brain death identification or with approval from the authorization committee.
The organ transplant process is a comprehensive review that is registered by a healthcare provider or medical professional and the administrative department of the transplant institution. The final approval is granted by the authorization committee.
What is the role of the transplant coordinator?
- Organ transplant coordinator is a multifaceted role which crucial for successful coordination between organ procurement and the transplant process. Deceased organ donation includes a close-knit network with many medical, paramedical, and non-paramedical personnel, with transplant coordinators. These transplant coordinators also known as procurement transplant coordinators or organ donor coordinators, are in this process.
- Organ donors are summoned when a potential organ donor meets specific criteria for donor allocation, such as severe neurological injury which leads to brain death determination. The transplant coordinator will review the donor’s medical records to start the process of placing organs with recipients if the donor is deemed suitable.
- The transplant coordinators manage the medical management to ensure the stability of the donor’s organ for transplantation. These donor coordinators are responsible for coordinating diagnostic tests which include blood tests for the donor’s blood typing and collaborate with providers to facilitate organ recovery for transplantation.
- The organ donation process and transplant programs’ success depend upon effective coordination with trained transplant coordinators.
- Transplant coordinators also provide support and counseling to donor families of brain-dead donors and encourage a positive environment for organ donation.
- After completing the process transplant coordinator helps in building strong relationships with both medical and non-medical communities, as well as families of deceased donors.
- Recipient transplant coordinators focus on educating patients about preparing for an organ transplant and post-transplant care of patients, to ensure the optimal outcomes for recipients.
What is the importance of a transplant coordinator?
The transplant coordinators help to identify the entire donation process from the brain death of a patient to the field of organ transplantation, which includes some important key responsibilities of a transplant coordinator:
- In the organ donation process transplant coordinators work closely with organ procurement organizations, transplant centers, and transplant hospitals to find potential organ donors, which also assess the donor suitability and coordinate the organ donation process from start to end.
- The role of transplant coordinators involves a complex structure, they are responsible for determining the potential organ donors after donor evaluation and help in clinical management or conventional management. It involves the process of assessing the organ functions and viability of medical history by gathering data, conducting physical examinations, or coordinating diagnostic tests to manage potential donors in intensive care units for optimal medical support and management.
- The process of organ donation includes a very crucial point of consent and communication in which the transplant coordinator’s role is to provide cooperation between donor families and support to donors’ families for obtaining consent or explaining the donation process to them.
- The transplant coordinator’s role provide support to the recipient and their families after the transplant surgery. They also assist in post-care management and follow-up appointments to promote optimal outcomes and ensure the continuity of care.
- Education and advocacy are important parts of this process in which transplant coordinators educate healthcare professionals, the public, and donor families to raise awareness about organ transplantation.
Deceased Transplant Coordinator vs Recipient Transplant Coordinator
A transplant coordinator and a recipient transplant coordinator have their respective roles in the organ donation and transplantation process. A transplant coordinator is also known as a deceased transplant coordinator; the primary role is to assist in the organ donation process from deceased donors. They work closely with donor families, healthcare professionals, and transplant teams to coordinate with organ procurement process, ensure patient suitability, and manage organ recovery and transportation.
Whereas a recipient transplant coordinator’s role is to coordinate care for the transplant recipient. They provide education to patients about the transplant process, coordinate with patients for transplant surgery, and provide support and post-transplant care.
Recipient transplant coordinators work with transplant teams, to ensure that recipients receive the necessary medical attention and follow-up care to optimize their outcomes after transplantation.
Important key points to be noted:
- A national system ensures fair distribution of donated organs based on medical needs and the medical urgency of the recipient’s condition. The procedure of organ allocation is followed by several factors, including the duration of time patients have spent on the organ transplant waiting list and the severity of their illness. This approach offers a chance for critically ill patients to survive so that life-saving organs reach those who need them the most.
- Between retrieval and transplantation, donated organs have a limited life span for viability. There are organ preservation techniques that maximize the life span of these organs after donation.
To learn more about continuous improvement in the field of critical care enroll in an Online Organ Donation Course.
Checklist for a Critical Care student to have a comprehensive understanding of the condition:
- Orientation to the Course: Organ Donation Simplified
- Defining Brain Death & THOA Law
- Selection of Cadaver Donor
- Brain Death Testing- How I Do It
- Concept of Brain Stem Death and Brain Stem Death Testing
- Medico-Legal Aspects of Cadaver Organ Donation
- Caveats in Brain Death
- Donor Optimization
- Ancillary Tests in Brain Death
- Role of the Transplant Coordinator in Organ Donation
Frequently Asked Questions (FAQs):
Q1. What’s the main barrier to organ donation?
Ans. Lack of open communication and public awareness. Many people don’t understand the process or feel uncomfortable discussing death.
Q2. What is the process of organ donation work in India?
Ans. Family consent is required to register as a donor after brain death. Organs are evaluated, matched with compatible recipients, retrieved, transplanted, and followed by aftercare for both the recipient and donor family.
Q3. What is the salary of the transplant coordinator in India?
Ans. In India transplant coordinator’s salary varies between Rs 0.9 Lakhs to Rs 9.0 Lakhs with less than 1 year of experience to 12 years, the average annual salary stands at Rs4.1 Lakhs.
Clearing MBBS is itself a difficult task and then cracking competitive exams is another level of challenge. But you can’t skip this challenging situation if you want to the accelerating graph of your career.
Success in the MRCP Part 1 exam signifies that you have not only retained the knowledge you learned during your undergraduate studies but that it has also grown to keep up with developments that have happened since you graduated and continues to serve as a foundation for clinical decision-making.
Most important to note, MRCP is just a pass or fail exam.
Step-by-Step Study Guide for MRCP Part 1 Exam
1. Understand the Exam Pattern.
MRCP Part 1 is a single-day Computer-based exam comprising two papers. Each paper has 100 multiple-choice questions to be solved in three hours. The MCQs follow the ‘best of five’ exam format. No negative marking gives a bit of relaxation for this competitive exam.
This MRCP Part 1 overview will let you get familiar with the exam pattern and will help you plan your preparation and revision strategy with effective time management. It is crucial to distribute the time to learn each specialty depending on the vastness of the subject, subject weightage, your level of understanding of the subject, etc.
Click here to learn the subject- weightage/blueprint of the MRCP Part 1 exam.
2. Choose your Exam Date Wisely.
It is advised to give the MRCP Part 1 first attempt after 12-24 months of graduation. Once you feel confident enough to take an exam, then only register for it. Usually, competitive exams are held once or twice a year, but the MRCP Part 1 exam occurs four times a year (January/April/August/October), which provides an opportunity for you to apply as per your suitability. You don’t have to wait for another year to sit the exam if you don’t want to sit for the exam this time.
3. Start Preparing Early.
Given how difficult the MRCP Part 1 test is, it’s crucial to give yourself plenty of time to study. Give a minimum of 6-10 months for sincere preparation. Don’t get confused; talk to seniors, faculty, friends, or mentors to get the best advice for you. Early preparation saves your time and boosts your confidence. Effective planning and consistency pave the way to effective results.
4. Make a Realistic Study Plan.
Create an MRCP Part 1 study plan that describes the material you will cover each day or week after you have your study materials. Allocate the time to a particular specialty keeping the factor in mind that your level of understanding is at beginner level or intermediate. Also, consider that there is enough time left for revision and practice questions. Revision strategy is also a must so that you don’t miss out on anything at the eleventh hour. Practice the question according to the exam pattern to get more familiar with it and this will also enhance your ability to tackle a question in the exam. Review your performance and revise your strategy accordingly.
5. Stick to Reliable Study Resources.
There are several options for MRCP Part 1 study materials, including books, online MRCP 1 exam resources, and question banks. To have a thorough grasp of the subject, it’s crucial to employ a range of materials, and resource selection is recommended. The preferred books for MRCP Part 1 are “Mastering Medicine: MRCP Made Easy” by Dr. Archith Boloor, Essential Revision Notes for MRCP by Philip A. Kalra, and the Oxford Handbook of Clinical Medicine by R.A. Hope. For online MRCP preparation may it be video lectures or Practice questions, you can subscribe to the ‘Cracking MRCP Part 1’ course. You can attend webinars and exam discussion videos only by the eminent faculty.
6. Enroll in online MRCP part 1 preparation courses.
To ace your MRCP preparation, you can enroll in one of the best online courses for MRCP Part 1, “Cracking MRCP Part 1” by eminent faculty, Dr. Gurpreet Singh Wander and Dr. Archith Boloor. The course covers modules covering all the major specialities and is devised based on The Royal College of Physicians curriculum. Every module in the Cracking MRCP Part 1 study materials includes webinars and video archives, approx. 2000 best of five MCQs/MRCP Part 1 practice questions, notes, high-yielding questions, e-chapters, and performance tracking. It additionally benefits you with the mock papers intended to give a feel of a real exam. The leaderboard ranking feature of the course enables you to track your performance and prepare accordingly. To ease the preparation and revision, the Cracking MRCP Part 1 notes are categorised into three sections: Wake-up calls, Golden signs, and Clinical gems. The Wake-up calls indicate the red flag signs pointing towards a certain disease or condition, Golden signs signify characteristic diagnostic features of a disease or condition, and Clinical gems signify recommended management or preferred drug choice for a disease or condition.
7. Don’t Miss Out on High-Weightage Topics.
A wide number of subjects are covered in the MRCP Part 1 exam; however, some are assessed more rigorously than others. The following are the high-weightage speciality/subjects:
- Cardiology
- Clinical Pharmacology and Therapeutics
- Clinical Sciences
- Endocrinology, Diabetes, and Metabolic Medicine
- Gastroenterology and Hepatology
- Infectious Diseases
- Neurology
- Renal Medicine
- Respiratory Medicine
- Rheumatology
8. Practice Mock Exams and Previous Year Papers.
Practicing mock exams and previous year’s papers is an excellent method to gauge your progress and determine where you need to concentrate and revise your strategy. There are a variety of mock tests accessible, both online and in books. DigiNerve with the Cracking MRCP Part 1 online course gives access to the free mock paper. You must attempt it under the timed condition for self-evaluation. Utilising question banks for practise will give you a better understanding of the questions that are asked.
9. Be Consistent and Manage Time Effectively.
Consistency is the key. Although taking the MRCP Part 1 test might be nerve-wracking, it’s crucial to remain composed and concentrated. Be consistent with your study routines along with balancing clinical practice.
Also, time management skills are crucial because the MRCP Part 1 test is timed. Give yourself enough time to respond to each question but avoid spending too much time on a single question. Mark the question for review if you are unsure about the answer, then go on. If you have time, you can return to the marked questions later. Remind yourself that you are prepared for the exam by taking deep breaths.
10. Take Good Care of your Health.
Consume healthful meals and get adequate sleep. Good health improves concentration and memory. Don’t get stressed a lot and meditate regularly because mental health is as important as physical health. Especially on the day of the exam, it’s critical to obtain adequate sleep and consume a balanced diet. You’ll be able to focus and remain awake as a result.
MRCP Part 1 Exam Day Tips
- Get familiar with the route and location of the exam centre and reach on time on exam day.
- Don’t be late for Paper-II after the break. It is advised to be at your desk at least 15 minutes before Paper-II is about the start.
- You are not allowed to take any items, accessories, or stationary along with you in the exam.
- The required stationery items are provided in the exam hall itself.
- Don’t wear hoods for the exam.
- Keep your ID handy for entry and checking purposes.
Frequently Asked Questions (FAQs)
Q1. What score do you need to pass MRCP Part 1?
Ans. The pass marks for MRCP Part 1 are around 540. The Equating process based on Response theory is used to calculate the candidate’s overall result. The pass marks are calculated as the overall scaled score unlike other exams, where the overall percentage score is considered.
Q2. Is there a negative marking in MRCP Part 1?
Ans. No, there is no negative marking in the MRCP Part 1. This is a great advantage for all the candidates aiming to clear the MRCP exam.
Q3. Is MRCP difficult to pass?
Ans. Undoubtedly, the MRCP exam is difficult to pass but not impossible. With smart study, consistent efforts, proper clinical practice, and effective time management, you can crack the MRCP exam.
The UPSC CMS is an abbreviation for “Union Public Service Commission-Combined Medical Services” Examination. It is a competitive examination that the Union Public Service Commission (UPSC) of India administers. The CMSE is held every year to fill various medical positions in government agencies including the Indian Railways, Central Health Service, Municipal Corporation of Delhi, and several other central government health institutions. The CMS exam allows medical professionals to join the esteemed Indian government healthcare service organizations and support the country’s healthcare system.
The difficulty level of the exam is self-explanatory by the term UPSC; UPSC CMSE is a hard nut to crack. With smart study, consistent efforts, and a lot of practice, you will pass with flying colours. Make sure to start early and stick to a realistic study plan and reliable study resources.
In this blog, you will get detailed information about the UPSC CMS exam recruitment category, eligibility criteria, exam pattern, selection procedure, and syllabus.
To be eligible to sit in the exam, a candidate must be either:
(a) an Indian citizen, or
(b) a subject of Nepal, or
(c) a subject of Bhutan, or
(d) a Tibetan refugee who came over to India before the 1st January 1962 to permanently settle in India, or
(e) a person of Indian origin who has migrated from Pakistan, Burma, Sri Lanka, or East African Countries of Kenya, Uganda, the United Republic of Tanzania, Zambia, 6 Malawi, Zaire, and Ethiopia or Vietnam to permanently settle in India.
Provided that a certificate of eligibility has been issued by the Government of India in favour of the candidate belonging to categories (b), (c), (d), and (e) mentioned above.
UPSC CMS Recruitment Category
UPSC CMS exam is conducted for the recruitment for the following categories and positions:
Category-I:
Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services
Category-II:
Assistant Divisional Medical Officer in the Railways
General Duty Medical Officer in New Delhi Municipal Council
General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
There are reservations for candidates belonging to Scheduled Castes, Scheduled Tribes, Other Backward Classes, Economically Weaker Sections, and Persons with Benchmark Disability as per the vacancies by the Government.
UPSC CMS Exam Pattern
Medical graduates with an MBBS degree along with completion of internship are eligible to apply for the UPSC CMS exam. There are two parts of CMSE, one is a written examination and the other is an interview. The CMSE comprises two theory papers followed by a personality test or interview. Here’s a breakdown of the exam pattern:
Part-I: Written Examination
The written examination comprises two papers:
Paper-I: This paper includes questions from General Medicine and Pediatrics subject. The exam Pattern 2024 for UPSC CMSE Paper-I is mentioned in the below table:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper I | 120 (96 questions from General Medicine and 24 from Pediatrics) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Paper-II: This paper includes questions from Surgery, Obstetrics & Gynecology, and Preventive and Social Medicine subjects. The Surgery subject also includes ENT, Ophthalmology, Traumatology, and Orthopaedics subjects. The table below mentions the exam scheme for UPSC CMSE Paper-II 2024:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper II | 120 (40 questions from each subject, Surgery, OBGYN, and Community Medicine) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Part-II: Interview/Personality Test
After passing the written test, candidates are invited by the Union Public Service Commission for an interview/personality test to determine their fit for the open positions.
The personality test carries 100 marks. The interview is designed to complement the written examination for measuring the general knowledge and academic study skills of the applicants as well as to function as a personality test to evaluate the candidate’s critical thinking skills, absorption capacity, and overall capacity for social cohesiveness, sound judgment, and moral character, initiative, and leadership potential. Basically, it aims to assess the candidate’s personality, communication skills, and suitability for the posts in medical services.
Final Selection
The final selection is done based on the combined marks obtained in Paper-I, Paper-II, and the Interview/Personality test.
Recruitment of a number of candidates is based on the vacancies in the particular position. Succeeding applicants are assigned to different Group-A positions within the public health system. The particular positions and openings change every year.
It’s significant to note that the Paper-I and Paper-II syllabuses contain a broad variety of medical science-related topics. A wide range of medical topics, including clinical disciplines, general knowledge, and current events, are covered in the CMSE curriculum. To score well on the test, candidates must have a solid comprehension of these topics. It is a crucial aspect of a good preparation strategy to know and understand the syllabus of the CMS exam. It leads to effective time management.
UPSC CMS Syllabus
UPSC CMS Syllabus Paper I:
General Medicine subject includes the following topics:
- Cardiology
- Respiratory diseases
- Gastro-intestinal
- Genito-Urinary
- Neurology
- Hematology
- Endocrinology
- Metabolic disorders
- Infections/Communicable Diseases
-
- Virus
- Rickets
- Bacterial
- Spirochetal
- Protozoan
- Metazoan
- Fungus
- Nutrition/Growth
- Diseases of the skin (Dermatology)
- Musculoskeletal System
- Psychiatry
- General
- Emergency Medicine
- Common Poisoning
- Snakebite
- Tropical Medicine
- Critical Care Medicine
- Emphasis on medical procedures
- Patho physiological basis of diseases
- Vaccines-preventable diseases and Non-vaccines preventable diseases
- Vitamin deficiency diseases
- In psychiatry – Depression, psychosis, anxiety, bipolar diseases, and Schizophrenia
Pediatrics subject includes the following topics:
- Common childhood emergencies
- Basic newborn care
- Normal developmental milestones
- Accidents and poisonings in children
- Birth defects and counselling including autism
- Immunization in children
- Recognizing and managing children with special needs
- National programmes related to child health
UPSC CMS Syllabus Paper II:
Surgery subject includes the following topics:
- General Surgery
- Wounds
- Infections
- Tumours
- Lymphatic
- Blood vessels
- Cysts/sinuses
- Head and neck
- Breast
- Alimentary tract
-
- Oesophagus
- Stomach
- Intestines
- Anus
- Developmental
-
- Liver, Bile, Pancreas
- Spleen
- Peritoneum
- Abdominal wall
- Abdominal injuries
- Urological Surgery
- Neurosurgery
- Otorhinolaryngology/E.N.T.
- Thoracic surgery
- Orthopaedic surgery
- Ophthalmology
- Anaesthesiology
- Traumatology
- Diagnosis and management of common surgical ailments
- Pre-operative and post-operative care of surgical patients
- Medico-legal and ethical issues of surgery
- Wound healing
- Fluid and electrolyte management in surgery
- Shock pathophysiology and management
Obstetrics and Gynecology subject includes the following topics:
- Questions on applied anatomy
- Questions on applied physiology of menstruation and fertilization
- Questions on infections in the genital tract
- Questions on neoplasm in the genital tract
- Questions on displacement of the uterus
- Normal delivery and safe delivery practices
- High-risk pregnancy and management
- Abortions
- Intra Uterine growth retardation
- Medicolegal examination in OBGYN including the rape
Family Planning subject includes the following topics:
- Conventional contraceptives
- D. and oral pills
- Operative procedure, sterilization, and organization of programmes in the urban and rural surroundings
- Medical Termination of Pregnancy
Preventive Social & Community Medicine subject include the following topics:
- Social and Community Medicine
- Concept of Health, Disease and Preventive Medicine
- Health Administration and Planning
- General Epidemiology
- Demography and Health Statistics
- Communicable Diseases
- Environmental Health
- Nutrition and Health
- Non-communicable Diseases
- Occupational Health
- Genetics and Health
- International Health
- Medical Sociology and Health Education
- Maternal and Child Health
- National Programmes
- Management of common health problems
- Ability to monitor national health programmes
- Knowledge of maternal and child wellness
- Ability to recognize, investigate, report, plan, and manage community health problems including malnutrition and emergencies.
You can also enroll in online MBBS courses to get conceptual clarity over MBBS subjects by the top medical faculty of India. You have the opportunity to learn and get your concepts clear in Surgery by Dr. Sriram Bhat M, Microbiology by Dr. Apurba S Sastry, Dr. Sandhya Bhat and Dr. Deepashree R, Medicine by Dr. Archith Boloor, Pathology by Prof Harsh Mohan, Prof Ramadas Nayak, and Dr. Debasis Gochhait, and similarly other MBBS subjects by subject’s eminent faculty. The comprehensive knowledge of MBBS subjects and problem-solving capabilities will directly impact your CMS exam.
Frequently Asked Questions (FAQs):
Q1. Is UPSC CMS conducted every year?
Ans. Yes, the UPSC CMS exam is conducted every year and the recruitment is based on the number of vacancies for a particular post in various government health organizations.
Q2. What is a career after CMS?
Ans. UPSC CMSE is conducted for the recruitment of the Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services, Assistant Divisional Medical Officer in the Railways, General Duty Medical Officer in New Delhi Municipal Council, and General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
Q3. Who conducts the CMS exam?
Ans. The CMS exam is a competitive examination conducted by the Union Public Service Commission (UPSC) of India.
Q4. What is the pattern of UPSC CMS exam?
Ans. There are two parts of CMSE in which part-I is a written examination and the part-II is an interview. The CMSE comprises two theory papers followed by a personality test or interview.
The Part-I written examination comprises two papers: Paper-I and Paper-II.
The National Medical Commission (NMC) has achieved the coveted World Federation for Medical Education (WFME) Recognition Status for a tenure of 10 years. This is a prestigious achievement for India’s medical education. This esteemed award proves NMC’s steadfast dedication to the highest standards in medical education and accreditation.
The WFME recognition will now enable Indian medical graduates to pursue postgraduate training and practice in other countries that require WFME recognition, such as Australia, USA, Canada, and New Zealand.
The World Federation for Medical Education (WFME) is a global organization dedicated to raising the standard of medical education all over the world. The WFME accreditation programme is crucial in ensuring that medical institutions uphold and adhere to the highest levels of global education and training standards.
Dr. Yogender Malik, Member of the Ethics and Medical Registration Board and Head Media Division at NMC, on this remarkable achievement, said, “WFME’s recognition underscores that the quality of medical education in India adheres to global standards. This accolade empowers our students with the opportunity to pursue their careers anywhere in the world, while also making India an attractive destination for international students due to our globally recognized standards.”
Under this accreditation, all the 706 existing medical colleges in India will be considered WFME accredited, and the new colleges being set up in the coming 10 years will also be considered as WFME accredited. This will also benefit NMC in enhancing the quality and standards of Indian medical education by aligning them with global benchmarks. This will facilitate academic collaborations and promote continuous improvement and innovation in medical education.
Now NMC being WFME accredited has opened the doors for all the medical students for ECFMG and USMLE. All Indian students will become eligible to apply for the Education Commission on Foreign Medical Graduates and United States Medical Licensing Examination.
The National Medical Council, Ministry of Health and Family Welfare in a press release dated 20th September 2023 has announced this remarkable update.
Global health comprises the biological and clinical facets of diseases along with the social, economic, political, and environmental determinants of health. The ability to confine health issues inside national borders has diminished as the globe becomes more linked.
The contribution of technology to the medical sector is unparalleled. With the years passing by technology is improving at the highest pace in the medicine sector. Nowadays, the use of AI, and the development of new therapies, drugs, drug development, and surgical procedures, have made complex medical procedures less complex and paved a path to minimally invasive surgeries. Millions of individuals throughout the world are having their lives improved as a result of these developments.
Global health has improved recently despite several obstacles like poverty, pandemics, disease outbreaks, conflicts, and climate change. Maternal and child fatalities have dropped significantly and since the development of new vaccinations, infectious illness spread has also been reduced. Governments and organisations have also boosted their funding for global health concerns and also significantly invested in newer technologies. The current developments in the healthcare industry are beneficial to global health and are an area with significant potential to enhance the health of people all over the world and in the medical field. We can improve the health of people all across the world by addressing the issues and embracing the possibilities.
Medical students and professionals must keep themselves updated and knowledgeable about the recent advancements in healthcare as it is going to impact their career growth to a great extent. To escalate the growth of your medical career, it is mandated to upskill.
The recent advancements in the global healthcare and medicine field are significant for several reasons. By offering more precise diagnoses, earlier illness detection, and more individualised treatment regimens, they have the potential to:
- Improve the quality of care for patients.
- By enabling remote monitoring and care and minimising the need for in-person visits, healthcare may be made more accessible and cheaper.
- Increase the effectiveness of healthcare delivery by simplifying administrative procedures and facilitating information exchange between healthcare professionals.
- Develop novel therapies and preventative measures to lessen the impact of chronic illnesses.
- Boost public health by keeping track of and rapidly and efficiently addressing illness outbreaks.
Below mentioned are technological advancements in medicine and global healthcare:
Artificial Intelligence and Healthcare
With the introduction of unprecedented tools for patient care, treatment, and diagnosis, artificial intelligence (AI) is drastically changing the healthcare industry.
For researchers interested in global health, AI-driven health interventions fall into four categories: diagnosis, patient morbidity or mortality risk assessment, disease outbreak prediction and surveillance, and health policy and planning. Machine learning, signal processing, data mining, natural language processing, and other forms of AI are applied in the healthcare sector.
Here are a few current applications of AI in healthcare:
- Diagnosis and treatment: Artificial intelligence (AI) paves the way for the screening of disease and can analyse medical images like X-rays and scans to identify illnesses early and more accurately than humans. AI may be used to create individualised treatment regimens for individuals based on their unique traits and requirements. Other applications of artificial intelligence being used in medicine include Digital chest radiographs, cervical cancer screening, estimating perinatal risk factors, and characterising and predicting the global spread of the Zika virus.
- Drug discovery: Artificial intelligence (AI) may be used to search through extensive databases of chemicals and compounds to find possible new medicines. AI may also be used to foresee how pharmaceuticals would react in the body, lowering the possibility of adverse effects.
- Personalised medicine: Artificial intelligence (AI) may be used to examine a patient’s genetic information, medical history, and lifestyle choices in order to develop a personalised treatment plan that has the highest chance of success.
- Risk assessment: AI may be used to predict the risk of disease and figure out how likely a patient is to have cancer or heart disease. Patients can utilise this knowledge to guide lifestyle adjustments that will lower their risk.
- Healthcare administration: AI may be used to automate processes like appointment scheduling, patient record management, and claim processing. This might free up medical personnel to concentrate on treating patients.
- Telemedicine: Platforms that employ AI in telemedicine can be used to offer doctor consultations via the Internet. Patients with limited access to healthcare in remote locations may particularly benefit from this.
- Robotics: Surgery, pharmaceutical dispensing, and other medical services can be carried out by AI-powered robots. This might aid in enhancing the effectiveness and precision of healthcare delivery.
- Big data analytics: Using AI, enormous databases of healthcare data may be analysed to spot trends and patterns. The diagnosis and treatment of illnesses can be made better with the use of this knowledge.
- Virtual assistants: AI-driven virtual assistants may be used to set up appointments, answer patients’ inquiries, and offer information about their conditions. The patient experience may be enhanced as a result of this.
The future of AI in healthcare is very promising. The use of AI in healthcare is still in its early stages, but it has the potential to revolutionize the way we diagnose, treat, and manage diseases. In the years to come, as AI technology advances, it is anticipated to have a more significant influence on the healthcare industry.
Advances in Gene Editing Technology
The science of gene editing is expanding quickly. The way we treat illnesses is changing as a result of gene editing tools like CRISPR-Cas9. These technologies can be used to fix genetic flaws that lead to disease or to add new genes that can offer disease protection.
The following are some of the developments in gene editing technologies that are being investigated for medical applications:
- CRISPR-Cas9: A protein called Cas9 is used by CRISPR-Cas9 to cut DNA at a precise spot. This enables precise gene replacement, deletion, and insertion. The most popular gene editing technology, CRISPR-Cas9, is being researched for a number of uses, including the treatment of HIV, cystic fibrosis, sickle cell disease, and hereditary illnesses.
For instance, in cancer patients, CRISPR-Cas9 is being utilised to create novel cancer medicines that can target and eliminate cancer cells. CAR T-cell treatments, a sort of immunotherapy that employs a patient’s immune cells to combat cancer, are being developed by researchers utilising CRISPR-Cas9.
- Base editing: A more recent gene editing technique, base editing allows you to alter specific DNA nucleotides without actually cutting the DNA. Compared to CRISPR-Cas9, this makes it less likely to result in unwanted side effects. For the therapy of conditions including cystic fibrosis and Duchenne muscular dystrophy, base editing is being researched.
- RNA editing: An approach to gene editing that can target RNA molecules rather than DNA. This can be utilised to treat conditions like certain cancers that are brought on by RNA alterations.
- Gene therapy: Gene therapy is a treatment that involves introducing genes into cells to correct a genetic defect. Numerous illnesses, including cancer, HIV, and hereditary ailments, have been treated by gene therapy.
These are only a handful of the gene editing innovations that are being investigated for medical applications. Technology’s continued advancement will probably have a significant influence on how we manage diseases in the years to come.
Development of Precision Medicine
A person’s unique genetic makeup, lifestyle, and environment are all taken into consideration when developing a medical treatment plan in precision/personalised medicine. This may result in a more effective and targeted treatment with fewer adverse effects.
Personalising medicine may be done in a variety of ways. Typical strategies include:
- Genetic testing includes examining a person’s DNA to see if there are any mutations or variances that might impact their likelihood of contracting a certain disease or their reaction to a particular medication.
- Biomarkers are quantifiable indications of a biological condition or state. Biomarkers can be used to monitor a patient’s response to therapy or to spot those who are most likely to catch a particular disease.
- Environmental factors, such as pollutant exposure, food, and exercise impact how people respond to therapy as well as the development of many diseases.
Precision medicine is becoming more and more feasible as we understand more about the human genome and the part genetics plays in disease. We can create more effective and focused therapies that may result in improvement by taking into consideration a person’s particular demands.
Here are some examples of current applications of precision medicine:
- High-risk cancer patients are identified via genetic testing, and targeted medicines are created that are more efficient for those who have certain genetic alterations.
- Biomarkers are being utilised to monitor an individual’s risk of developing heart disease and to pinpoint those who will benefit from certain therapies the most.
- Scientists are examining the genetic component of Alzheimer’s disease and creating targeted treatments that might be more efficient for those who carry particular genetic abnormalities.
Some of the challenges and limitations of precision medicine include cost, accuracy, accessibility, and regulation.
Personalised medicine is a promising subject with the potential to enhance millions of people’s lives despite these difficulties. It is anticipated to become more accessible, inexpensive, and accurate as technology advances.
Development of Telemedicine and Remote Healthcare
Telemedicine and remote healthcare allow patients to receive care from a doctor or other healthcare provider without having to travel to a doctor’s office or hospital. This can help with healthcare access, particularly in remote locations. The COVID-19 pandemic has spurred telemedicine and remote healthcare development to a great extent. These services are increasingly enticing to patients and providers alike because of the requirement to maintain social distance and avoid in-person visits to healthcare institutions. There are several advantages to telemedicine and remote medical care, such as better access to healthcare, lower healthcare expenses, increased patient satisfaction, and better patient results.
Remote healthcare services and telemedicine come in a wide variety. The most popular ones are Tele-education, remote patient monitoring, and virtual doctor appointments.
Additionally, there are several drawbacks to telemedicine and remote treatment, such as security and privacy issues, a lack of financing, technical issues, and a shortage of skilled providers.
Despite these impediments, telemedicine and remote healthcare are expanding quickly and playing a bigger role in the healthcare system. These services are expected to become progressively more common and available as technology advances.
Here are some of the future trends in telemedicine and remote healthcare:
- Increasing the use of artificial intelligence (AI): AI may be applied to personalise treatment regimens, increase the precision of diagnoses, and keep track of patient’s health.
- Development of novel telehealth technology: More thorough and individualised treatment will be feasible thanks to new gadgets like wearable sensors and virtual reality headsets.
- Expansion into new areas: Telemedicine and remote healthcare will be utilised to deliver care in new areas, such as managing chronic diseases and mental health.
Application of 3D Printing in Healthcare
3D printing in medicine is being used to create customised medical items including prostheses, implants, and surgical guides. This innovation might save expenditures while raising the standard of treatment. A rapidly developing technology, 3D printing has a wide range of potential uses in the healthcare sector. Among the most widespread applications of 3D printing in the medical field, some are mentioned below:
- Producing patient-specific medical devices: 3D printing may be used to produce personalised medical items like implants, prostheses, and surgical guides that are tailored to the anatomy of a single patient. In addition to lowering the risk of problems, this can enhance the device’s fit and functionality.
- Building medical models and educating healthcare professionals: 3D printing may be used to build accurate representations of the human body’s organs, tissues, and tumours. These models can be used to aid in the planning and execution of intricate treatments as well as the education of patients about their conditions. This can assist them in picking up new abilities and methods, as well as in practising approaches in a secure setting.
- Creating novel medications and treatments: Tissue scaffolds for cell culture and intricate drug delivery systems may be made using 3D printing. This can aid in the development of novel treatments and medications by researchers for a number of disorders.
- Customising care: Using 3D printing, it is possible to develop treatments and drugs that are specifically suited to the requirements of a certain patient. This might increase the therapy’s efficacy and security.
Here are some specific examples of how 3D printing is being used in healthcare today:
- A company named Materialise has created a 3D-printed breast implant that is specifically designed for women with tuberous breasts. This type of breast deformity is often difficult to treat with traditional implants, but the 3D-printed implant can provide a more natural and comfortable fit.
- A team of researchers at the University of California, San Diego has developed a 3D-printed surgical guide that can be used to remove brain tumors with greater precision and accuracy.
- A company named Organovo has developed a 3D printer that can be used to create human tissue. This tissue can be used to study diseases, develop new drugs, and create personalized medical implants.
These are some of the numerous uses for 3D printing that are now being made in the medical field. As technology advances, it will probably have a bigger influence on the healthcare sector, enhancing the standard of treatment and enhancing accessibility for all.
The use of blockchain technology to increase the security and effectiveness of healthcare data exchange is one of the significant developments being made in the world of healthcare. Smart technologies, particularly wearable sensors, are being developed to extract therapeutically significant health-related data from physical (body) indicators like heart rate, blood pressure, body temperature, respiration rate, and body motion. The technology has now also come up with immersive virtual and augmented reality training and education in the medical field.
Advancements in technology, increased investment in global health, partnerships, collaborations among the government, organizations, and individuals, and innovations altogether make a significant contribution to addressing the challenges to global health and improving health outcomes. The rapid pace of technical improvement has made these developments feasible. These technologies will have a bigger influence on global healthcare as they advance.
Chapter 3 of the NExT Exam 2023 update comprises the objective, distribution and level of questions, paper and distribution of subjects, and proposed schedule of both NExT step 1 and 2.
NExT Step 1
- Objective
This step is a computer-based exam with multiple choice questions aimed to ensure objectivity and address a higher level of knowledge assessing the competencies of a medical graduate.
- Distribution and knowledge level of Questions
- Majority of items must assess higher level comprehension, analytical skills, and clinical problem-solving that are in line with competencies to assure evaluation of higher domains of medical learning.
- The NExT Step 1 style is meant to discourage medical students from rote learning.
- Case studies and clinical case studies will make up the majority of the test; MCQ questions will be allocated roughly as follows across all subjects:
- Problem-solving and analytical skill types – 60% – 70%
- Comprehension type- 20% – 30%
- Recall type- 05% – 15%
- The level of knowledge necessary to get skills will be roughly
- Must Know: 60%
- Nice to Know: 30%
- May Know: 10%
- Pattern and Distribution of Subjects
- Six subject papers with corresponding weightage and time allocation will be included in the NExT Step 1 exam.
- Applied features of all other MBBS subjects, including forensic medicine and toxicology (FMT) as well as community medicine, will be mainstreamed within the pertinent clinical subjects.
- The subjects are listed below along with their appropriate item weightings and time allotments:
| Papers | Subjects | No. of Items | Duration |
| 1 | Medicine & allied subjects | 120 | 3.0 hours |
| 2 | Surgery & allied subjects | 120 | 3.0 hours |
| 3 | Obstetrics & Gynecology | 120 | 3.0 hours |
| 4 | Pediatrics | 60 | 1.5 hours |
| 5 | Otorhinolaryngology | 60 | 1.5 hours |
| 6 | Ophthalmology | 60 | 1.5 hours |
- Proposed Time Schedule of Papers
| Day | Subject | Duration | Break | Subject | Duration |
| 1 | Medicine & allied subjects | 3.0 hours | 2.0 hours | Paediatrics | 1.5 hours |
| 2 | No Examination | ||||
| 3 | Surgery & allied subjects | 3.0 hours | 2.0 hours | Otorhinolaryngology | 1.5 hours |
| 4 | No Examination | ||||
| 5 | Obstetrics & Gynaecology | 3.0 hours | 2.0 hours | Ophthalmology | 1.5 hours |
NExT Step 2
- Objective
This step shall be a clinical/practical examination to be conducted after the successful completion of the internship. The objective of this step is to evaluate the competencies of the medical graduates in clinical diagnosis, patient and clinical decision-making, and practical and communication skills.
- Evaluation Methods
The examination will comprise Actual cases, Objective Structured Clinical Examination (OSCE), and Simulations if possible.
There will only be two levels of grading available: “Competent” or “Pass”/”Not Competent” or “Fail” depending on the likelihood of satisfactory performance or unsatisfactory performance.
- Distribution of Subjects
The following subjects shall be evaluated during NExT Step 2:
- Medicine and allied subjects
- Surgery and allied subjects
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
- Orthopaedics and Physical Medicine & Rehabilitation (PMR)
- Time Schedule
The schedule and modalities of NExT Step 2 shall be decided by the National Medical Commission and the respective authorized Universities/Institutions after completion of the internship and the price of the admission process for the Postgraduate Courses of that year.
Time Schedule of NExT Examination and associated events
Proposed Time Schedule:
| S.No. | Event | Commencement Date of Exam | Completion Date |
| 1 | NExT Step I Regular | May/November | 1st week June/December |
| 2 | III MBBS /FINAL MBBS PART 2 Practical / Clinical University Examination | 1st Week June/December | 3rd Week June/December |
| 3 | Internship | 1st Week January/July
|
31st December/30th June of the following year |
| 4 | NExT Step 2 Regular | 3rd Week June/December | 4th Week June/December |
| 5 | NExT Step 2 Supplementary | 1st Week September/March | 3rd Week September/March |
| 6 | Post Graduate Admission | May-June (Counselling) | 30th June |
| 7 | Postgraduate Course | 1st July/1st Week January | — |
Click Here to Read NMC NExT Exam Update – Chapter 1 (Preliminary)
Click Here to Read NMC NExT Exam Update – Chapter 2 (Broad Outline)
The Chapter 2 of the NMC Update describes the broad outline of the National Exit Exam, including general features of steps 1 and 2, NExT scores, nature of scores, minimum passing score, etc.
General Features of the NExT Exam
The NExT Exam shall comprise two separate exams referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
NExT Step 1
1.NExT Step 1 shall be a theoretical and Computer-based/Online examination.
2. It shall comprise one or more types of multiple-choice questions.
3. This shall be a Centralized Common All India Examination that will be held by a body designated by the commission as the conducting authority.
4. The examination shall include six papers covering topics from both Part 1 and 2 of the III MBBS/Final MBBS programme:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
(Applied aspects of all subjects covered under I MBBS and II MBBS and Applied aspects of all subjects covered under III MBBS/Final MBBS Part l)
5. Students who have completed their III MBBS/Final MBBS course from a recognized medical college shall be eligible to appear for the examination.
6. NExT Step 1 Examination shall be held twice a year in the months of May and November tentatively.
7. There shall be no restriction on the number of attempts to participate in NExT Step 1 provided that the candidate has completed both the NExT Step 1 and NExT Step 2 exams within ten years of enrolling in the MBBS Course.
8. There is no cap on the number of times for attempting the NExT Step 1 Regular Examination to improve your score but you can only go for the improvement after completing your NExT Step 2.
9. The III MBBS/Final MBBS Part 1 and III MBBS/Final MBBS Part II Practical/clinical examinations will continue to be held conventionally unless otherwise stated by the Commission and the NExT Step 1 will replace the traditional university/institutional Theory Examinations of the III MBBS/Final MBBS Part II.
NExT Step 2
1. The NExT Step 2 shall be a Practical/Clinical and viva voce examination comprising seven clinical subjects/disciplines:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
- Orthopaedics and PMR (Physical Medicine and Rehabilitation)
2. The exam shall be objectively structured, clinical case-based, and use simulated cases and patients to evaluate practical and clinical skills as well as clinical decision-making and communication abilities expected of an Indian medical graduate.
3. The exam must be taken in person or live, and it must be administered by the relevant state health universities or institutions in accordance with the norms and directives given by the Commission. The Commission will choose the university or institution that is permitted to conduct NExT Step 2 for the relevant colleges where there are no state health universities.
4. The Regular NExT Step 2 Exam shall be held twice a year.
5. A NExT Step 2 Supplementary Examination is only open to candidates who have failed in one or more (up to three) of the seven subjects and are required to repeat specific subjects. It will be held twice a year. If a candidate fails in more than three subjects, then they will have to appear in supplementary exams of all the seven subjects.
7. As long as the candidate has completed both the NExT Step 1 and NExT Step 2 Examinations within ten years of enrolling in the MBBS programme, there is no restriction on the number of attempts to participate in NExT Step 2.
NExT Scores
1. Nature of Scoring
- The marks in NExT Step 1 must be calculated as a whole number, which will serve as the Raw Scores with the proper decimals. Also, equivalent Percentages (marks out of a maximum of 100) with the proper decimals may then be calculated.
- The outcomes of the NExT 2 exams will only be reported as Pass/Fail depending on the acquisition of the relevant competence that is being evaluated.
2. Minimum scores for passing
- The minimum score to pass shall be 50% of the total or half of the maximum possible Raw for NExT Step 1.
- To pass the NExT Step 1 exam, you must receive a minimum of 50% (50 out of 100) in each of the six papers or half of the maximum possible Raw Scores.
- The requirements for passing NExT Step 2 include a successful demonstration of having acquired the competencies that are evaluated, with a pass/fail result being given.
3. Calculation of NExT Step 1 scores for determining merit for the purpose of admission to Postgraduate courses in broad specialties
- The sum of the raw scores earned in each paper or topic in a single NExT 1 exam will be used to calculate the Total Marks for determining the merit, particularly for admission to broad specialization Postgraduate Courses.
- The candidate must follow the generation of a rank application process as stipulated by the Commission from time to time in order to determine rank for admission into Postgraduate courses in broad specializations in a given academic year. Only individuals who have submitted an application for rank generation will be eligible for admission for that cycle of the academic year.
- The NExT Step results will be valid for five years in order to determine merit, notably for admission to broad-specialty postgraduate courses. If a candidate has appeared in the NExT exam cycle then the score of the latest given NExT step 1 exam will be considered.
- Tie-breaker rule for rank generation:
-
- Normalized sum of raw scores obtained in each paper in NExT step 1 although the method of normalization will be notified later.
- Candidate with the lower attempts in NExT step 1 will be placed higher in the merit list.
- Candidates will be given higher rank based on the higher marks in the following order of preference:
-
-
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
-
4. Utility of NExT Scores
- An MBBS student from a college recognized by the Commission shall be eligible for compulsory internship only if they pass in each of the six theory papers of NExT Part 1 and also pass in III MBBS/Final MBBS (Part 2) Practical/Clinical Examination.
- A medical student who has completed their undergraduate studies abroad at an institution recognized by the Commission and who has met the necessary requirements outlined in the Commission’s Foreign Medical Graduate Regulations is eligible to participate in the mandatory rotating internship programme only if they pass in all six NExT Step 1 Theory Papers.
- A medical graduate who received their training in India or outside of India will be entitled to register in the Indian Medical Register and State Medical Register and obtain a license to practice modern medicine in India, only if, they have completed the internship for the appropriate length of time and have successfully passed the NExT Step 2 (Practical / Clinical) Examination. You must fulfill all the requirements as per the Registration of Medical Practitioners and Licence to practice Medicine Regulations, of NMC. Also, all the other requirements are considered appropriate by the Commission, Concerned University/Institution and duly applicable at that time.
- For admission to PG medical courses in broad specialty subjects, a candidate must meet the following criteria:
- Candidates must meet the conditions outlined for NExT Part 1 and 2, making them eligible for a license to practice modern medicine in India.
- Must engage in common counselling by a designated authority granted by the Central Government or Commission.
- The NExT Step I Scores may be used by the Government of India, the State Governments, any organization of the Government of India, the State Governments, or any autonomous or private body/institution for the purpose of employment, provided that the necessary authorization has been sought and authorized by the National Medical Commission or other appropriate authorities as determined to be appropriate.
Click Here to Read NMC NExT Exam Update – Chapter 1 (Preliminary)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
The NExT Exam latest news includes Chapter 1 (Preliminary) and Chapter 2 (Broad Outline) and Chapter 3 (General Information).
The core objective of the NExT exam is to provide consistency in summative evaluations conducted across the nation in relation to the minimal requirements for a medical graduate’s education and training.
The National Exit Test (NExT), shall serve as a licentiate examination for validating a medical graduate’s eligibility to register for practice the contemporary system of medicine in India.
NExT will also act as an entrance exam for admission to PG medical education in broad medical specialties by determining the eligibility and ranking of the MBBS students.
The National Exit Exam shall be applicable to:
- All undergraduate medical students seeking the MBBS degree at all medical colleges that have been accredited by the National Medical Commission along with Institutes of National Importance (INIs) are subject to the National Exit Test (NExT).
- All foreign medical graduates who have been granted approval by the NMC for the purposes of obtaining a license to practice medicine as a registered medical practitioner in India and for enrollment in the State Register or the National Register in such a manner as may be specified by regulations.
- Anyone with a medical degree aiming to pursue an academic course, an observership, or any other purpose that may be specified and allowed by the NMC by appropriate notification or rules from time to time.
- Anyone with the granted medical license practicing in India wishes to pursue PG degree can take the NExT exam.
According to the draft released, the NExT comprises two separate examinations, referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
The Commission shall from time to time determine, by appropriate regulations and/or notification, the applicable method of employing the NExT results for admission to Postgraduate Courses in wide medical specialties by means of common counselling by the designated authority.
There is no confirmation yet on the academic session to which the NExT exam will be applicable but when it will come into force, all other corresponding and equivalent examinations shall be phased/ceased out.
It is still to be decided by the Commission Central Government, State Government, that the existing examinations, however, shall continue for as long as may be necessary or the analogous existing exams will be replaced by the NExT. The Commission will decide when it is necessary and will notify the use of scores and normalization of various examinations and the NExT, when applicable concurrently, for such purposes as may be appropriate.
Chapters 2 and 3 of the update include the complete structure of the NExT Examination, objectives, exam pattern, eligibility, distribution of subjects, nature of scoring, timetables, and more.
Click Here to Read NMC NExT Exam Update – Chapter 2 (Broad Outline)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
The MRCOG Part 3 clinical assessment aims to evaluate applicants’ aptitude for applying fundamental clinical abilities about the skills, knowledge, attitudes, and competencies outlined in the MRCOG Part 2 curriculum. One receives membership in the Royal College of Obstetricians and Gynecologists after passing the MRCOG Part 3 exam (MRCOG).
Eligibility for MRCOG Part 3
- To be eligible for Part 3, the aspirant must have passed the MRCOG Part 2 and got the Assessment of Training (AoT) approved.
- For AoT, 4 years of training in Obstetrics and Gynecology is required, of which 2 years should be within the 4 years preceding the candidate’s initial application.
Assessment of Training (AoT)
- It is a prime requirement to register for the MRCOG Part 3 or the MTI scheme.
- After completing the MRCOG Part 1 exam, you can only apply to have your training evaluated. AoT can also be filled before the Part 2 results.
- Applications for AoT can be made at any time, but you can’t take the MRCOG Part 3 exam until your application has been approved.
- Processing of AoT application takes up to 4 weeks.
- Candidates who already met the MRCOG Part 2 eligibility requirements, including having their Assessment of Training certified before July 2019, do not need to reapply.
AoT Deadlines
| Part 3 MRCOG exam | Deadline for AoT |
| Part 3 MRCOG exam- February 2023 | 24 October 2022 |
| Part 3 MRCOG exam- May 2023 | 26 January 2023 |
| MTI 2023 | 31 October 2022 |
Post-registration Training
There are two ways that post-registration training is evaluated to determine eligibility for the Part 3 MRCOG exam:
Route A: Applicable only for learners in a reputable UK specialized training programme.
Route B: Applicable for all other candidates.
Route A
Participants in an accredited specialist training programme in the UK should show evidence of the following:
- At the time of applying for the Assessment of Training, the applicant must be enrolled in intermediate training at the ST3 level or higher.
- The National Training Number must be included in the application for AoT that trainees must submit.
- There is no need for any supporting documents; if the college needs more information, candidates will be notified via email after receiving their application.
Route B
Candidates who are not enrolled in an approved specialized training programme in the UK should exhibit the following:
- A minimum of 4 years of full-time experience in obstetrics and gynecology or an equivalent post-registration position in the UK or abroad.
- Within the 4 years before a candidate’s initial application, he/she must spend at least 2 years (full-time or equivalent) in the specialty.
- A single post must have been held for at least six months straight.
- All foreign O&G hospital-based positions are welcomed.
- When applying the AoT, training must be finished.
- Flexible training in recognized positions is allowed as long as College approval is obtained in advance.
MTI 2023 Scheme
Medical Training Initiative (MTI)
International Medical Graduates (IMGs) can go to the UK under the MTI scheme for up to 2 years to train in the National Health Service (NHS). They must fulfill all the eligibility criteria and apply for the same.
MRCOG Part 3 Exam Pattern
The MRCOG Part 3 Clinical Assessment comprises 14 tasks in a circuit based on the 14 modules from the syllabus.
The duration of each task is 12 minutes including 2 minutes of initial reading time.
The assessment for the MRCOG Part 3 is done in the context of five domains:
- Patient safety
- Communication with patients and their relatives
- Communication with colleagues
- Information gathering
- Applied clinical knowledge
Types of Tasks
The MRCOG Part 3 contains two different types of tasks:
- Simulated patient/colleague tasks: The candidate will interact with a patient (actor) who has been prepared and well-prepped for the role they will play during the simulated patient/colleague tasks. The actor will be well-versed in the pertinent case information and will be prepared with some pre-written questions to ask if required.
- Structured discussion tasks: These tasks require the candidate to communicate directly with a clinical examiner. To prevent the candidate from running out of time, the examiner will have a list of questions and comprehensive instructions for the work that they can use to prompt the candidate. As the scenario develops, the examiner could provide the candidate with additional knowledge before posing new questions.
- A circuit may have “linked tasks,” wherein the second task is coupled to the first, to allow for more depth in the assessment of applied clinical knowledge. There can also be assignments where candidates need to write something.
How many attempts are allowed for the MRCOG Part 3?
In MRCOG Part 3, candidates are allowed 4 attempts. Candidates must retake the MRCOG Part 2 exam if they are unsuccessful after four attempts.
This does not, however, count as an attempt for candidates taking the digital remote exam for the first time.
MRCOG Part 3 Exam Date
The MRCOG Part 3 is conducted in three sessions per year.
The February 2023 MRCOG Part 3 exam is a supplemental test outside of MRCOG’s regular schedule to give the international O&G community one more opportunity to obtain an exam spot. This exam is specifically designed to give applicants outside of the UK another opportunity to take the MRCOG Part 3 exam.
February 2023 Exam Important Dates
| Deadline for all candidates to ensure the home address and email address is up to date | 2 December 2022 (Friday) |
| Closing Date for Assessment of Training | 24 October 2022 (Monday) |
| Opening Date for Booking window application | 8 December 2022 (Thursday) |
| Closing Date for Booking window application | 19 December 2022 (Monday) |
| Exam Dates | 6th – 9th February 2023
8th – 12th May 2023 6th – 10th November 2023
|
| Result Declaration | 7 March 2023 (Tuesday) |
Aspirants can apply for training assessment after passing MRCOG Part 1 exam.
MRCOG Part 3 Examination Fee
| Location | Fees (2023) |
| UK and Republic of Ireland | £563 |
| Band A | £901 |
| Band B (India comes under this category) | £840 |
| Band C | £617 |
Points to Note for the fee structure:
- India comes under Band B. Thus, the fee for the candidates having exam centres in India is £840 which is equivalent to INR 73,584.37. The amount in the Indian currency varies as per the currency change.
- Payments are linked to the country’s bandings of international membership fees.
- Banding applies to the center where you take the exam, not the candidate’s country of residence.
- You can check out on the official website under which band your exam centre country falls.
MRCOG Part 3 Pass Marks
RCOG Procedure: The standard for determining whether a candidate is competent is determined using this approach, which is based on adding the number of examiner judgments in a specific examination to an additional factor and a standard measurement error.
MRCOG Part 2 is a written examination aimed at assessing the application of knowledge of medical aspirants in clinical scenarios.
MRCOG Part 2 Exam Pattern
- MRCOG Part 2 is a computer-based test.
- The CBT consists of two papers. Both papers are worth the same number of points, hence, paper 1 and paper 2 each account for 50% of the final grade. There are two different question types on each paper:
- Single-Best Answers (SBAs) account for 40% of the final grade.
- Each question includes the following:
- A lead-in statement, i.e., question.
- A-E represents the five options on the list.
- There is no negative marking.
- Incorrect answers are marked zero.
- Extended Matching Questions (EMQs) account for 60% of the final grade.
- Each question includes a lead-in statement, which tells you clearly what to do with a list of 10-14 possible options to choose from.
- Even though it may seem like there are multiple options, you must only select the option with the highest likelihood.
- There is no negative marking.
Timetable of MRCOG Part 2
| Paper 1 and Paper 2 | |
| Particulars | Description |
| Duration | 3 hours (180 minutes) for each paper |
| Number of questions | 50 SBAs and 50 EMQs for each paper |
| Lunch break (approximately one hour) between both the papers | |
Time Management Tip: The RCOG advises devoting 110 minutes to EMQs and 70 minutes to SBAs.
Distribution of Marks
The SBAs and EMQs share a single pass mark. There is a composite pass grade that is established by establishing standards for each exam.
A total of 40% of the final grade is determined by the SBA component, and 60% is determined by the EMQ component. As a result, applicants must devote roughly 40% of their time to the SBA component and roughly 60% to the EMQ component.
How to Apply for MRCOG Part 2?
Eligibility of MRCOG Part 2
- In order to be eligible to sit for the MRCOG Part 2 exam, candidates must first pass the MRCOG Part 1 exam.
- Candidates who have passed the Part 1 MRCOG after March 2013 need to attempt the Part 2 MRCOG within 7 years of their exam date.
- To enter to UK Specialist register, you must clear both part 1 and part 2 within 6 attempts only.
How many times are you allowed to retake each test?
No matter when they make their first attempt, candidates are only allowed a total of 6 chances to pass the MRCOG Part 1 and Part 2 tests.
How to book the MRCOG Part 2 exam?
- Expression of Interest
Candidates are required to fill Expression of Interest form, within the stipulated time.
- MRCOG Part 2 Exam Calendar
The MRCOG Part 2 exam is conducted twice a year, one of which is on 17th January 2023 and the other on 5th July 2023.
a.
| Closing Date for Expression of Interest form | 14 October 2022 (Friday) |
| Opening Date for Booking window application | 10 November 2022 (Thursday) |
| Closing Date for Booking window application | 15 December 2022 (Thursday) |
| Exam Date | 17 January 2023 (Tuesday) |
| Result Declaration | 21 February 2023 (Tuesday) |
b.
| Closing Date for Expression of Interest form | 16 March 2023 (Thursday) |
| Opening Date for Booking window application | 27 April 2023 (Thursday) |
| Closing Date for Booking window application | 09 June 2023 (Friday) |
| Exam Date | 05 July 2023 (Wednesday) |
| Result Declaration | 01 August 2023 (Tuesday) |
MRCOG Part 2 Examination Fee
| Location | Fees (2023) |
| UK and Republic of Ireland | £523 |
| Band A | £631 |
| Band B (India comes under this category) | £544 |
| Band C | £434 |
Points to Note for the Fee Structure:
- India comes under Band B. Thus, the fee for the candidates having exam centres in India is £544 which is equivalent to INR 54,285.67. The amount in the Indian currency varies as per the currency change.
- Payments are linked to the country’s bandings of international membership fees.
- Banding applies to the center where you take the exam, not the candidate’s country of residence.
- You can check out on the official website that in which band your exam centre country falls under3. Choose a Country and Book into the Pearson VUE test centre
After the successful submission of the Expression of Interest form, candidates will receive an email regarding the opening date of the application window.
Candidates will then have to choose the examination country and pay the required exam fee. Then the candidates will be asked to select the Pearson VUE test centre in the respective country they have chosen and paid for.
MRCOG Part 2 Pass Marks
The standard setting is done to ensure fair examination and to accurately determine the candidate’s performance. The pass marks and the pass rate vary according to exam sitting as there is no fixed level or quota.
Angoff Method: The Angoff Method entails the evaluation of each question by a group of subject matter experts (O&G Consultants in NHS practice), who then estimate the likelihood that a borderline applicant would know the answer. The final pass mark is calculated by averaging these estimates and adding them to the measurement standard error. A measurement of an assessment’s accuracy is its standard error of measurement. It serves as a function of both the standard deviation of observed results and the test’s reliability and reveals the degree of variability in a test given to a group.
Linear Equating: In order to guarantee identical standards across subsequent examination diets, the linear equating method is used. By assessing and comparing candidate performance on a small number of “anchored” (repeated) and un-anchored questions, this technique adjusts for the relative difficulty of the papers by comparing the current results to those of previous diets.
How long should you wait to take the following MRCOG Part?
- Candidates who passed the MRCOG Part 1 after March 2013 must retake the exam within seven years after the MRCOG Part 2 exam date.
- The seven-year period is pro rata. This indicates that for trainees enrolled in less than full-time training or who take a break from training, the 7-year duration is proportionally extended, up to a maximum of 10 years.
- Candidates who passed Part 1 of the MRCOG in March 2013 or earlier must sit for Part 2 of the MRCOG within 10 years of passing Part 1.
- Candidates who complete Part 2 of the MRCOG must take Part 3 of the MRCOG within 7 years (prorated) of the Part 2 exam date.
- The amount of time between attempts for the MRCOG Part 2 or Part 3 is not limited.
- It is possible to take the Part 1 MRCOG before beginning UK specialist training.
- The MRCOG Part 2 must be taken within 10 years of the exam date of the candidate’s passed MRCOG Part 1 if they do not desire to be included in the UK Specialist Register.
There is no time limit on how frequently applicants may retake MRCOG Part 2 or Part 3 if they do not want to be added to the UK Specialist Register.
To get conceptual clarity with the help of MBBS Courses Online, Click Here.
The Membership of the Royal College of Physicians (MRCP) is a postgraduate diploma in internal medicine in the United Kingdom. It’s a valuable qualification as it’s an internationally recognized diploma and is the shortest route to a career in medicine around the world. The exam tests students on their knowledge of basic medical sciences as well as the clinical skills required for the diagnosis and management of diseases. The MRCP is recognized in countries around the world, and valued especially in the UK, the UAE, Singapore, and Ireland. The MRCP is also recognised by UAE’s board and opens up opportunities to practice in the Middle East as well.
The MRCP is challenging and preparing for it takes months, since students usually take it while pursuing their post-graduation, but the advantages of obtaining a MRCP degree makes the pressure worthwhile. You cannot sit the MRCP exam without having completed 12 months of medical experience by the date of the examination, as the MRCP focuses on the real world applications of medical knowledge, measuring not just your theoretical knowledge, but your practical skills as well. It is designed to test your competence in medicine overall.
Once you have the certification, you can work as a consultant physician in a private hospital in India. However, another advantage of passing the MRCP medical exam is its recognition abroad.
All you need to know about MRCP Examination & MRCP Full Form
MRCP is the Membership of the Royal Colleges of Physicians of the United Kingdom. The exam is conducted for doctors who are interested in receiving higher specialty training from the Royal College of Physicians of Edinburgh, the Royal College of Physicians and Surgeons of Glasgow, and the Royal College of Physicians of London. It is a set of three exams designed to test the knowledge, skills, and behavior of clinicians in training.
MRCP(UK) is conducted in three parts:
- MRCP Part 1 (Written Examination)
- MRCP Part 2 (Written Examination)
- MRCP Part 2 Clinical Examination (PACES)
MRCP (UK) studies play an important role in the overall educational experience and continuing professional development of doctors in the UK and internationally. An MRCP (UK) Diploma is required for doctors who wish to undergo training in the medical specialty in the United Kingdom. The MRCP exam is a globally recognized qualification that is seen as an excellent benchmark against which doctors are judged on their competence and suitability for specialist training.
How to apply for the MRCP exam 2023?
- Register online through My MRCP (UK) official website.
- Make sure to recheck all the details you have mentioned.
- At this point, you will be required to submit evidence of primary medical qualification (PMQ).
- After the basic registration, go to the Upcoming exams section and apply for the respective exam type you want to appear for (Part 1/2/PACES).
- Mention the details if you are training in UK or not.
- Choose a country and city as your examination center.
- Fill out the details in the special arrangement section if required.
- Pay the applicable examination fee.
- Your application is confirmed via an automatically generated email.
- Candidates who have limitations in their practice should fill out an online declaration form with the application itself.
Mode of MRCP Exam
The exam is conducted in two modes:
- Online mode: The exam is conducted in online mode using an online proctored system for candidates within the UK and the Republic of Ireland. The students appearing for the online exam will have to fulfill all the criteria as per the organization and read the guidelines including the online exam procedure, IT setup, important points to know before and after the exam, and other exam regulations and codes of conduct.
- Offline mode: The rest of the candidates from different countries including India will have to give the exam in the offline mode. Offline exams are conducted at exam centers in various countries. However, the exam center is different for the MRCP Exam part 1 & 2 and PACES.
The content and format of the exam are the same for both modes so the preparation should be done in the same way.
Read out further to get the complete information about all the three parts of the MRCP exam.
MRCP Part 1
Aim of MRCP Exam Part 1
- It is an entry-level exam.
- The purpose of the MRCP Part 1 is to test the understanding of basic clinical sciences that a medical graduate is expected to comprehend.
- Part 1 exam is designed to assess students’ knowledge of clinical science and prevalent and significant illnesses as described in the UK curriculum.
- Additionally, you’re tested on the most important and commonly encountered diseases from several specialties.
MRCP Exam Eligibility
Medicos from any part of the world can give the exam. Candidates with a medical degree from an institute recognized by GMC (General Medicine Council), followed by 12 months of medical employment after your graduation are eligible to apply for the exam.
Candidates are required to send proof/evidence of completion of their medical degree along with at least 12 months of medical employment.
MRCP Part 1 Exam Dates
MRCP 1 is conducted 4 times a year. The 2022/4 exam will be held on 30th Nov 2022 and the result will be declared on 11th January 2023.
Exam Schedule for MRCP Part 1 Exam 2023
| 2023 Session | Application Period | Exam Date | Result Date |
| 1st (2023/1) |
7 Nov 2022 – 14 Nov 2022 | 25 Jan 2023 | 8 Mar 2023 |
| 2nd (2023/2) |
13 Feb 2023 – 20 Feb 2023 | 19 Apr 2023 | 31 May 2023 |
| 3rd (2023/3) |
29 May 2023 – 5 Jun 2023 | 9 Aug 2023 | 13 Sep 2023 |
| 4th (2023/4) |
14 Aug 2023 – 21 Aug 2023 | 18 Oct 2023 | 29 Nov 2023 |
MRCP Part 1 Exam fees
- For part 1, the examination fee is £460 for UK students.
- For international students including India, the exam fee is £616, which approximately amounts to 59,904.20 Indian Rupee. The amount in INR can vary depending on the currency difference.
MRCP Part 1 Exam Pattern
- It is a single-day examination.
- It consists of two papers of 3 hours duration each.
- Each paper has 100 questions.
- MCQ pattern with the ‘best of five options’ type questions.
- There is no negative marking.
- There are no image-based questions.
Subject weightage in MRCP Part 1
The exam comprises questions from the various specialties:
| Specialty | Number of questions |
| Cardiology | 14 |
| Clinical Pharmacology and Therapeutics | 15 |
| Clinical Sciences | 25 |
| Dermatology | 8 |
| Endocrinology, diabetes and metabolic medicine | 14 |
| Gastroenterology and Hepatology | 14 |
| Geriatric medicine | 8 |
| Hematology | 10 |
| Infectious diseases | 14 |
| Neurology | 14 |
| Oncology | 5 |
| Medical ophthalmology | 4 |
| Palliative medicine and end of lifecare | 4 |
| Psychiatry | 9 |
| Renal medicine | 14 |
| Respiratory medicine | 14 |
| Rheumatology | 14 |
| TOTAL – 200 |
The Clinical Sciences portion will include questions from the following specialties:
| Specialty | Number of questions |
| Cell, molecular, and membrane biology | 2 |
| Clinical anatomy | 3 |
| Clinical biochemistry and metabolism | 4 |
| Clinical physiology | 4 |
| Genetics | 3 |
| Immunology | 4 |
| Statistics, epidemiology, and evidence-based medicine | 5 |
Marking System for Part 1 and Part 2 Written Examination
An “Equating method” is used for calculating a candidate’s overall score. This procedure is statistically based on item response theory and utilized to guarantee equivalent outcomes for candidates in the test for equivalent performance on various diets.
All candidates are given an “overall scaled score” instead of an overall percentage score. The grade is calculated based on the number of questions answered correctly in the two test papers of the exam and takes into account the relative difficulty of the exam.
Note:
- For every correct response, a +1 mark is awarded.
- There is no negative marking in the MRCP written exam.
- If a candidate opts for more than one correct response or the answer is not correctly marked, then the marks awarded to the candidate are zero.
Passing Marks
As per the last academic session, the qualifying score for MRCP Part 1 exam is 540 marks. You need to get at least these many marks to qualify for MRCP Part 1 and become eligible for the MRCP part 2 written exam.
MRCP Part 2
Aim of MRCP Exam Part 2
In this exam, the capacity of the doctors to use clinical knowledge, form clinical judgments, and assume accountability will be evaluated.
Factors evaluated in MRCP Part 2:
- Putting issue or diagnostic lists to prepare an investigation
- Choosing a strategy for emergency management
- Choosing a long-term management strategy
- Determining prognosis
MRCP Part 2 Eligibility
To be eligible for Part 2, the candidate must have successfully passed the MRCP Part 1 written exam within the preceding 7 years.
A candidate will have to re-appear for the Part 1 written exam if he/she could not pass the MRCP Part 2 written or PACES exam within 7 years of passing the MRCP part 1 exam.
MRCP Part 2 Exam Dates
The MRCP exam is also conducted 4 times a year. The 2022/4 part 2 exam will be held on 14th December 2022 and the result will be declared on 25th January 2023.
Exam Schedule for MRCP Part 2 Exam 2023
| 2023 Session | Application Period | Exam Date | Result Date |
| 1st (2023/1) |
21 Nov 2022 – 28 Nov 2022 | 22 Feb 2023 | 05 Apr 2023 |
| 2nd (2023/2) |
13 Mar 2023 – 20 Mar 2023 | 17 May 2023 | 28 Jun 2023 |
| 3rd (2023/3) |
03 Jul 2023 – 10 Jul 2023 | 06 Sep 2023 | 18 Oct 2023 |
| 4th (2023/4) |
18 Sep 2023 – 25 Sep 2023 | 22 Nov 2023 | 03 Jan 2024 |
MRCP Part 2 Exam fees
- For UK students, the examination fee is £460.
- For international students including India, the exam fee is £616, which approximately amounts to 59,904.20 Indian Rupee. The amount in INR can vary depending on the currency difference.
MRCP Part 2 Exam Pattern
- It is a single-day examination.
- It consists of two papers of 3 hours duration each.
- Each paper has 100 questions.
- MCQ pattern with the ‘best of five options (BOFs)’ type questions.
- There is no negative marking.
- These include image-based questions, unlike Part 1.
Subject weightage in MRCP Part 2
For the theoretical questions, you can expect the following pattern of distribution
| Specialty | Number of questions |
| Cardiology | 19 |
| Clinical Pharmacology and Therapeutics | 18 |
| Dermatology | 9 |
| Endocrinology, diabetes and metabolic medicine | 19 |
| Gastroenterology and Hepatology | 19 |
| Geriatric medicine | 9 |
| Haematology | 9 |
| Haematology | 10 |
| Infectious diseases | 19 |
| Neurology | 17 |
| Oncology | 6 |
| Medical ophthalmology | 3 |
| Palliative medicine and end of lifecare | 3 |
| Psychiatry | 3 |
| Renal medicine | 19 |
| Respiratory medicine | 19 |
| Rheumatology | 19 |
| TOTAL – 200 |
For the image-based questions, you can expect questions from:
- Clinical photographs
- Pathology slides
- Inheritance trees
- ECGS
- X-rays
- CT and MR scans
- Echocardiograms
In the Part 2 exam, the questions are usually based on clinical scenarios and may be illustrated images. There can be questions related to the diagnosis, investigation, management, and prognosis of patients.
Passing marks
454 marks are considered a qualifying score for part 2. After you have cleared your MRCP part 2, you can proceed toward your MRCP Part 2 Clinical Examinations, i.e., PACES.
The MRCP Part 1 and Part 2 examination are both written exams and have almost the same pattern, but the PACES exam is entirely different from both parts. It has a completely different pattern and evaluation procedure.
MRCP Part 2 Clinical Examination (PACES)
PACES, abbreviated for Practical Assessment of Clinical Examination Skills, is designed to examine the clinical knowledge and acumen of doctors who wish to enter advanced training (ST3).
Aim of the PACES Exam
You are desired to know each of the following clinical skills:
- Clinical examination
- Identifying physical signs
- Clinical communication
- Differential diagnosis
- Clinical judgment
- Managing patient concern
- Maintaining patient welfare
Eligibility for MRCP PACES
The eligibility for PACES is the same as is for MRCP 2, i.e, you must have cleared your MRCP part 1 within the last 7 years.
MRCP PACES Exam Date
It is conducted 3 times a year, from January to March, June to August, and September to December.
The dates for the PACES exam are different for the UK and other countries and even for different centers.
MRCP PACES Exam Pattern
It is a half-day examination that takes place at hospitals or clinical centers.
There are five clinical positions (Stations) staffed either by patients with a specific disease or by trained support staff (surrogates). Each station has two independent examiners who observe and evaluate the candidates’ performance.
You can start at any station and move to the next station every 20 minutes until you complete the cycle. There is a 5-minute break between each station.
The five stations are allotted for the following:
- Respiratory, Abdomen
- History taking
- Cardiovascular and Nervous system
- Communication skills
- Brief clinical consolation
At least 4 weeks before your examination date, admission documents with your assigned examination date, time, and location will be sent.
Application Process
All the candidates are advised to read all the instructions carefully before filling out the application form.
2023 Application dates for the UK
| 2023 Session | Application Period | Assessment Period |
| 1st (2023/1) |
14 Nov 2022 – 21 Nov 2022 | Late January – March |
| 2nd (2023/2) |
27 Mar 2023 – 03 Apr 2023 | Early June – Early August |
| 3rd (2023/3) |
24 Jul 2023 – 31 Jul 2023 | Late September – Early December |
2023 International Application Period
| 2023 Session | Application Period |
| 1st (2023/1) |
10 Oct 2022 – 17 Oct 2022 |
| 2nd (2023/2) |
20 Feb 2023 – 27 Feb 2023 |
| 3rd (2023/3) |
19 Jun 2023 – 26 Jun 2023 |
In the 2023 International Application Period, the assessment period is not yet released.
Exams are not scheduled for each day of the assessment period, and exam schedules differ amongst colleges. Your exam date and venue will be listed in your admissions application.
MRCP PACES Fees
- For UK students, the examination fee is £657.
- For international students including India, the exam fee is £1202, which approximately amounts to 1,16,891.00 Indian Rupee. The amount in INR can vary depending on the currency difference.
Marking System for MRCP Part 2 Clinical Examination (PACES)
The candidates are assessed based on their clinical skills in this part of the exam. The exam process is as follows:
- Five clinical stations are set up with either trained stand-ins or patients with a specific disease (surrogate patients).
- There are two separate examiners at each station.
- For prospects to succeed, the candidate must achieve a minimum standard in each of the seven competencies as well as a minimum overall score.
Passing marks in PACES
You need to pass each clinical station separately based on clinical standards. Additionally, a minimum of 130 out of 170 is required to pass the PACES.
Let’s read some relevant information for all the parts of MRCP.
Number of attempts for the MRCP Exam
A maximum of six attempts are allowed at each part of the MRCP (UK) diploma. If any candidate wants to appear after six attempts, then for each re-exam, they must have undertaken additional educational experience. A candidate will also have to submit a form along with evidence of the additional educational experience, supported by the candidate’s Educational Supervisor and the Training Programme Director or equivalent.
MRCP Exam Centre
MRCP (UK) exams can be taken anywhere in the world. Candidates have the option of giving MRCP (UK) written exams at 34 international locations and the MRCP (UK) Clinical Examination (PACES) at 16 different locations.
MRCP Exam Centre in India
For Parts 1 and 2:
- Chennai
- Hyderabad
- Kerala
- Kolkata
- Mumbai
- New Delhi
For PACES:
- Bengaluru
- Chennai
- Hyderabad
- Kochi
- Kolkata
- New Delhi
- Pondicherry
- Thiruvananthapuram
Language requirements
- The MRCP exam (all parts) is conducted in English language only.
- The candidates are advised to have a command of the English language equivalent to a 7.5 band score in the IELTS exam. However, no language exam is required to be eligible for the MRCP exam.
Examining Board
There are examination boards for the MRCP (UK) Part 1, MRCP (UK) Part 2 Written, and MRCP (UK) Part 2 Clinical (PACES) exams. The examining board for PACES is also referred to as the Clinical Examining Board (CEB). Its task is to ensure the scientific quality of the examinations, which includes approving the content and determining the passing grade. The examination boards also deal with appeals, cases of scientific or professional misconduct, and complaints.
Withdrawal and Refund
Any candidate who wishes to withdraw his/her application should contact the appropriate administrative office by email and complete all the withdrawal procedures. They must mention the following details in the email for identity verification such as RCP code number, full name, and date of birth. The withdrawal application will not be counted as an attempt.
The withdrawal request must be submitted before the application process ends, so that a refund of 90% can be generated. A 10% application fee is deducted as an administrative charge.
Completion of MRCP Diploma
Once a candidate completes the last component of the diploma successfully, a results letter that attests to their success is given. Details about membership elections and entrance ceremonies is included in this email.
Right time to take your MRCP Exam
In general, data suggests that candidates have the highest pass rates when the candidates
- take the first part 1 exam attempt within 12-24 months of graduation
- take the first part 2 exam attempt within 36 months of graduation
- take the first part 2 clinical exam (PACES) attempt at least after 36 months of graduation
- Pass the Part 2 written exam before taking PACES.
- Before applying for PACES and completing the exam, it is advised to at least have 2 years of core medical training experience. A candidate should involve in emergency medical patient care for at least 4 months in the 2-year tenure of medical practice.
The information here will help you make the best choice about when to take the exam.
Points to note:
- Candidates are not allowed to apply through any third-party organization.
- After passing Part 1, candidates are ineligible to retake the exam until the 7-year window is passed.
- A candidate must complete both Part-2 written and clinical within seven years after the MRCP part 1 exam.
- A candidate is advised to attempt the mock test available on the MRCP UK official website.
- Before taking any of the examinations, candidates are highly encouraged to become familiar with the contents of these publications:
- MRCP (UK) Regulations (updated August 2022)
- Specialty Certificate Examination Regulations
- European Specialty Examination Regulations
- Examination Appeals Regulations
- Examination Complaint Procedure
- Reasonable Adjustments Procedure
- Code of Conduct
- Misconduct Regulations
If you want the opportunity of working abroad in the UK, the Middle East, Australia, Singapore, and many other countries, then the MRCP is the best qualification to have. The MRCP is a prerequisite to anyone wishing to go on to a specialist training post as a physician in the United Kingdom and in Australia. In the UAE, the MRCP is considered a super speciality degree, and consequently, those who have taken the MRCP are paid at par with super specialists. Doctors who pass the MRCP Exam can apply to jobs in any country that recognizes the degree abroad. Most countries welcome people who have professional degrees and can add value to the country and help its citizens. If you’re a doctor, you have a higher chance of being granted a work visa than most other jobs. If you think at some point you may want to live abroad, the MRCP is by far the best qualification to have.
DigiNerve is an e-learning platform by Jaypee which offers information and online coaching courses for the MRCP exams.
Frequently Asked Questions (FAQs)
-
Is there any online course for preparation for MRCP Part 1?
Ans: For cracking your MRCP 1, you have the strongest preparation available on DigiNerve, prepared by the eminent faculty of medicine, Dr. Archith Boloor and Dr. Gurpreet Singh Wander. The course is based on The Royal College of Physicians’ curriculum (RCP). There are 15 online modules in the course, which includes content on major disciplines including Clinical Sciences, Cardiology, Gastroenterology, etc. It also includes high-yield questions, mock papers, e-chapters, video lectures, notes and BOFs.
-
How many stages does MRCP has?
Ans: It is a set of 3 exams designed to test the knowledge, skills, and behavior of clinicians in training.
- MRCP Part 1 Written Examination
- MRCP Part 2 Written Examination
- MRCP Part 2 Clinical Examination (PACES)
-
How much is the MRCP exam fees?
Ans: The fees for MRCP Part 1 and 2 (Written):
- £460 (UK)
- £616 (International)
The fees for MRCP Part 2 Clinical Examination (PACES):
- £657 (UK)
- £1202 (International)
-
How many attempts do you get at MRCP?
Ans: A maximum of six attempts are allowed for each part of the MRCP (UK) diploma. If any candidate wants to appear after six attempts, then for each re-exam, they must have undertaken additional educational experience.
INI-CET is a combined national-level entrance examination for admission to the medical postgraduate courses – MD, MS, DM (6 yrs), MCh (6 yrs), and MDS at INI institutes (Institute of National Importance). The INI-CET January session 2023 exam is around the corner. Getting admission to INI institutes is highly challenging and a dream for MBBS students. This is a highly competitive task to secure a seat in the renowned medical colleges in India.
Remember, Perseverance is the key.
The INI-CET exam is going to be held on 13th Nov 2022 for admission to the AIIMS INI-CET January session 2023.
Mode and Scheme of INI-CET January 2023 exam
| Particulars | Description |
| Mode of Examination | Computer-based test (CBT) |
| Duration | 3 hours (180 minutes) |
| Number of questions | 200 |
| Types of questions | Objective type |
| Marking Scheme | +1 mark for every correct response and -1/3 for every incorrect response |
Important things to know:
- If more than one candidate scores the same, then this tie-breaker situation is resolved by applying the following criteria sequentially:
-
- Less negative marks
- Older by age
- Candidates equal to 8 (eight) times the number of postgraduate seats available in each category will be called for the first and second rounds of seat distribution based on the INI-CET merit list.
- Spot Round Counseling will only be conducted if the seats will remain vacant even after the open round counseling.
List of Participating Institutes for INI-CET January 2023 Session
| S. No. | Name |
| 1 | AIIMS, New Delhi |
| 2 | AIIMS, Bhopal |
| 3 | AIIMS, Bhubaneswar |
| 4 | AIIMS, Jodhpur |
| 5 | AIIMS, Nagpur |
| 6 | AIIMS, Patna |
| 7 | AIIMS, Raipur |
| 8 | AIIMS, Rishikesh |
| 9 | AIIMS, Bibinagar |
| 10 | AIIMS, Bhatinda |
| 11 | AIIMS, Deoghar |
| 12 | AIIMS, Mangalagiri |
| 13 | AIIMS, Raebareli |
| 14 | JIPMER, Puducherry |
| 15 | NIMHANS, Bengaluru |
| 16 | PGIMER, Chandigarh |
| 17 | SCTIMST, Trivandrum |
Here’s the tentative seat distribution (Category-wise) for admission to various MS/MD/DM (6 years)/MCh (6 years)/MDS courses at AIIMS, New Delhi and other 12 AIIMS through the INI-CET entrance examination for the January session of 2023.
Table 1: Tentative seat distribution for INI-CET January 2023 session at AIIMS, New Delhi:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 17 | 7 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Biochemistry | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Biophysics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Community Medicine | 9 | 5 | 2 | 1 | 0 | 1 |
| MD | Dermatology & Venerology | 5 | 1 | 2 | 1 | 0 | 1 |
| MD | Emergency Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Geriatric Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Lab. Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Medicine | 11 | 5 | 3 | 2 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 4 | 3 | 0 | 0 | 0 | 1 |
| MD | Obstetrics & Gynecology | 11 | 4 | 3 | 2 | 1 | 1 |
| MD | Ophthalmology | 6 | 3 | 1 | 1 | 1 | 0 |
| MS | Orthopaedics | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Otorhinolaryngology | 5 | 1 | 1 | 1 | 1 | 1 |
| MD | Pediatrics | 10 | 3 | 3 | 2 | 1 | 1 |
| MD | Palliative Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Pathology | 10 | 4 | 3 | 1 | 1 | 1 |
| MD | Pharmacology | 6 | 1 | 2 | 1 | 1 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Physiology | 10 | 5 | 2 | 1 | 1 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Radiodiagnosis & Internventional Radiology | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiation Oncology | 4 | 3 | 1 | 0 | 0 | 0 |
| MS | Surgery | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Transfusion Medicine | 5 | 2 | 2 | 1 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MDS | Pediatrics & Preventive Dentistry | 2 | 0 | 1 | 0 | 0 | 1 |
| MDS | Prosthodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MCh | Neuro Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Paediatric Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Infectious Diseases DM(Direct 6 year Course) | 4 | 4 | 0 | 0 | 0 | 0 |
Table 2: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhopal:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 1 | 0 | 1 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynecology | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Ophthalmology | 3 | 1 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | Pathology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 0 | 0 | 1 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine & Blood Bank | 2 | 0 | 0 | 1 | 1 | 0 |
Table 3: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhubaneswar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 9 | 3 | 2 | 2 | 1 | 1 |
| MD | Anatomy | 7 | 3 | 2 | 2 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Dermatology | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Emergency Medicine | 5 | 2 | 1 | 1 | 1 | 0 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | General Medicine | 3 | 2 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Obst. & Gynecology | 6 | 3 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 6 | 4 | 1 | 0 | 0 | 1 |
| MD | Pediatrics | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Pathology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Physiology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | PMR | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 0 | 1 | 1 | 1 |
| MD | Radiodiagnosis | 3 | 2 | 0 | 0 | 1 | 0 |
| MD | Radiotherapy | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Transfusion Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
Table 4: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Jodhpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology & Critical Care | 17 | 6 | 5 | 3 | 1 | 2 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Community Medicine | 6 | 2 | 2 | 1 | 1 | 0 |
| MD | Dermatology & Venerology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Emergency Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | General Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | General Surgery | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Microbiology | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | Otorhinolaryngology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | Paediatrics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Pathology | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physiology | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | PMR | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Radiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Transfusion Medicine & Blood Bank | 2 | 1 | 1 | 0 | 0 | 0 |
| MCh | Paediatric Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Radiation Oncology (D.M. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
Table 5: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Patna:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 18 | 8 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 3 | 1 | 0 | 1 | 0 |
| MD | Biochemistry | 9 | 4 | 3 | 2 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 8 | 3 | 2 | 1 | 0 | 2 |
| MD | Dermatology | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | ENT | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Emergency Medicine | 7 | 2 | 2 | 2 | 0 | 1 |
| MD | FMT (Forensic Medicine & Toxicology) | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Medicine | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | OBG (Obstetrics & Gynaecology) | 5 | 1 | 1 | 0 | 2 | 1 |
| MD | Ophthalmology | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Orthopaedics | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Pediatrics | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pathology | 5 | 0 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 3 | 0 | 0 | 0 | 0 |
| MD | Physiology | 7 | 4 | 2 | 1 | 0 | 0 |
| MD | PMR | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Radiodiagnosis | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiotherapy | 2 | 0 | 2 | 0 | 0 | 0 |
| MS | Surgery | 5 | 2 | 1 | 1 | 0 | 1 |
| MCh | Pediatric Surgery (MCh 6 Years) | 3 | 3 | 0 | 0 | 0 | 0 |
Table 6: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raipur:
| Course | Subject/Specialty | Total Number of seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 13 | 4 | 4 | 2 | 1 | 2 |
| MD | Anatomy | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Community Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Dermatology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Emergency Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MS | ENT | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 9 | 4 | 3 | 1 | 0 | 1 |
| MS | General Surgery | 8 | 3 | 3 | 1 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 7 | 2 | 1 | 2 | 0 | 2 |
| MD | Ophthalmology | 8 | 4 | 2 | 1 | 1 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pediatrics | 7 | 3 | 1 | 1 | 1 | 1 |
| MD | Pathology | 8 | 4 | 2 | 2 | 0 | 0 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physical Medicine & Rehabilitation | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Physiology | 2 | 0 | 1 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 1 | 0 | 0 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Pediatric and Preventive Dentistry (MDS) | 1 | 0 | 1 | 0 | 0 | 0 |
Table 7: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Rishikesh:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 7 | 3 | 2 | 1 | 0 | 1 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 2 | 0 | 0 | 1 | 1 |
| MD | Community & Family Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Dermatology & Venerology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Emergency Medicine | 3 | 2 | 0 | 1 | 0 | 0 |
| MS | ENT | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Geriatric Medicine | 1 | 0 | 1 | 0 | 0 | 0 |
| MS | General Surgery | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Nuclear Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Ophthalmology | 6 | 4 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pathology | 5 | 3 | 1 | 1 | 0 | 0 |
| MD | Pharmacology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Physiology | 3 | 2 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiation Oncology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Respiratory Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MDS | Periodontics (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MCH 6 Years | Pediatric Surgery (MCH 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Plastic, Reconstructive & Burns Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Neurosurgery (MCH 6 yrs) | 1 | 1 | 0 | 0 | 0 | 0 |
Table 8: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Nagpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine | 3 | 1 | 2 | 0 | 0 | 0 |
| MD | Dermatology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 0 | 2 | 0 | 0 | 1 |
| MS | General Surgery | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Ophthalmology | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Otorhinolaryngology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Pediatrics | 3 | 0 | 1 | 0 | 1 | 1 |
| MD | Pathology | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics (MDS) | 0
|
0 | 0 | 0 | 0 | 0 |
Table 9: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bibinagar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | FMT | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 2 | 1 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Peediatrics | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Pathology | 2 | 1 | 0 | 0 | 0 | 1 |
Table 10: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bathinda:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Ophthalmology | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 0 | 1 | 0 | 0 | 0 |
Table 11: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Deoghar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | FMT | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Pathology | 1 | 1 | 0 | 0 | 0 | 0 |
Table 12: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Mangalagiri:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Table 13: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raebareli:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Last-Minute Tips for INI-CET Exam:
- Candidates must carry all the asked documents such as INI-CET admit card, passport size photograph, valid photo ID proof, and a copy of MCI registration certificate with them on the exam day.
- Reverify all your documents before coming to the exam hall.
- Candidates are advised to go through all the guidelines issued by AIIMS for the examination.
- Candidates must reach the INI-CET exam center before time to avoid any chaos.
- Avoid Stress and be confident.
- Eat healthy and sleep well.
- Time management is a must before and during the exam.
To get conceptual clarity on the MBBS courses online, click here
The National Medical Commission (Undergraduate Medical Education Board) has issued new guidelines and the academic calendar for MBBS 2022-2023 batch on 12th Oct 2022.
As per the new NMC guidelines, the classes for the first-year MBBS batch will start on 15th Nov 2022.
Academic Calendar for the 2022-2023 MBBS Batch
According to the new NMC guidelines, there is a change in the academic calendar of MBBS 2022-2023. However, the duration of the MBBS course is the same i.e., 5.5 years including a one-year rotational internship.
| Professional Year | Time Frame | Subjects | Months(Teaching + Exam + Results) |
| 1st | 15th Nov’22 to 15th Dec’23 | Anatomy, Physiology, Biochemistry | 13 months |
| 2nd | 16th Dec’23 to 15th Jan’25 | Pathology, Microbiology, and Pharmacology | 13 months |
| 3rd (III-part-1) | 16th Jan’25 to 30th Nov’25 | Forensic Medicine and Toxicology, Community Medicine/PSM | 10.5 months |
| 4th (III-part-2) | Dec’25 to May’27 | General Surgery, General Medicine, Pediatrics, Obstetrics & Gynecology, ENT, Ophthalmology |
17.5 months |
| Internship | 1st Jun’27 to 31st May’28 | As per the CRMI 2021 Regulations | 12 months |
| PG | 1st Jul ‘28 |
For the academic year 2022-2023, the one-year compulsory rotational internship will start from the 1st June 2027 and end on 31st May 2028, as per the CRMI 2021 regulations.
The following guidelines have been issued by the NMC for the 2022-23 MBBS batch:
- The MBBS batch will commence on 15th Nov 2022.
- The college vacations and examination schedules may be notified as per the affiliated universities of the respective colleges.
Other board guidelines are as follows:
- Regarding Electives – 2 blocks of 15 days each are to be adjusted by the colleges for
- Pre/para-clinical branches
- Clinical branches
- In the 2022-2023 academic batch, the supplementary exams will be conducted with a gap of 1 month from the regular exams and the results will be declared within 15 days.
- There shall be no supplementary MBBS batches.
- The remaining rules and regulations shall remain the same as per the GMER (Graduate Medical Education Regulations) 1997. You can visit the site for GMER 1997 details: https://www.nmc.org.in/rules-regulations/graduate-medical-education-regulations-1997/
- The Yoga and Family Adoption Program through village outreach shall continue for the 2021-2022 MBBS Batch.
Along with the changes in the curriculum and the guidelines mentioned above, a few more notifications have been issued by the NMC from the 2022 batch:
- The NMC has created an Anti-Ragging Committee and Dr. Aruna V. Vanikar, President, UGMEB has been appointed as the chairperson of the committee.
- In the NMC notification stated on 4 Oct 2022, the implementation of HMIS (Hospital Management Information System) is mandated in all medical colleges.
- The NEET UG counselling link is active from 11th Oct 2022 on the MCC official website: https://mcc.nic.in.
Click here to read about the NMC NExT Exam update 2023 including the guidelines, complete structure, exam dates and more.
Christian Medical College (CMC), Vellore is a private medical college, hospital, and research institute. CMC is one of the best private medical colleges in India. In and around Vellore, Tamil Nadu, India, this institute has a network of primary, secondary, and tertiary care hospitals. Dr. Ida Scudder is the founder of CMC Vellore. The college is affiliated with the Tamil Nadu Dr. M.G.R. Medical University, Chennai. CMC, Vellore is approved by NMC (National Medical Commission). It is ranked as one of the top medical colleges in India. The institution offers admission to various disciplines of sciences: medical science, nursing, allied health sciences, some other master’s and doctoral programs, and post-graduate engineering programs.
The college offers admission to various programs including:
- Undergraduate medical course (MBBS)
- Medical postgraduate courses (diploma, degree, and higher speciality courses)
- Certification courses
- Postdoctoral fellowship courses
- Distance education program
- Undergraduate nursing program
- Nursing postgraduate courses (diploma, degree, and fellowships)
- Allied health sciences degree courses
- MBA in hospital and health systems management (HHSM)
- MS Bioengineering
- Tech. Clinical Engineering
- D. Medical Sciences
MBBS in CMC Vellore
MBBS is a four-and-a-half-year course followed by one year compulsory rotating residential internship. In CMC, Vellore, the MBBS course comes under the group A category. As per the CBME curriculum, the undergraduate course in medicine comprises three phases.
Three phases in MBBS Curriculum
| Phases in MBBS Curriculum | Duration | Subjects Included |
| 1 (Pre-Clinical Phase) | 13 months | Basic Sciences, Anatomy, Physiology, Biochemistry, Introduction to Community Medicine, Humanities, and Professional Development |
| 2 (Para-Clinical Phase) | 12 months | Pharmacology, Pathology, and Microbiology |
| 3 (Clinical Phase) | Part 1: 13 months
Part 2: 13 months |
Forensic Medicine, Community Medicine, Ophthalmology, and Otorhinolaryngology.
Medicine and Allied Specialties, Surgery & Allied Specialties, Child Health, and Obstetrics & Gynecology. |
Block postings and Internship at CMC Vellore
As per the guidelines of the National Medical Commission,
- Along with regular classes, medical students also have to undergo block postings after phase 1 of their MBBS course at community health centers, mission hospitals, and secondary care centers.
- A medical student also has to compulsorily complete the rotational internship for 12 months. They are posted in the discipline of community health, medicine, surgery, obstetrics & gynecology, orthopaedics, emergency medicine, and short elective subjects.
- At CMC, Vellore, the students are allocated community health centers, mission hospitals, and secondary care centers for internships.
Admission procedure
Admission to the MBBS undergraduate course in CMC, Vellore solely depends on the NEET-UG score. An aspirant to get admission at CMC needs to qualify and crack the NEET-UG (National Eligibility cum Entrance Test) examination with a good score.
Eligibility to get admission at Christian Medical College
- Candidate must have completed 10+2 higher secondary schooling or equivalent examination, and the last two years of education must include Physics, Chemistry, and Biology/Biotechnology as major subjects with English from the Tamil Nadu State board or any other equivalent examination board.
- Candidates must have attained a minimum of 50% marks in all the subjects, Physics, Chemistry, Biology/Biotechnology, and English individually for the general category, and a minimum of 40% aggregate for BC, MBC, SC/ST candidates is required in a single attempt. The criteria mentioned are subject to change as per the state & university guidelines.
- At the time of admission, a candidate must have completed 17 years of age or should complete the mentioned on or before 31st December of the said year.
NEET-UG Exam Pattern for admission to MBBS at CMC Vellore
The NEET-UG exam is conducted by National Testing Agency (NTA) once a year. The following are some important points to keep in mind:
| Particulars | Description |
| Exam Mode | Offline (pen & paper based) |
| Type of Examination | Multiple choice questions |
| The total number of questions | 200 questions (180 MCQs must be answered) |
| NEET total marks | 720 marks |
| Marking scheme | +4 for each correct answer and -1 for every incorrect answer |
| Total duration | 3hrs 20 mins |
| Languages | The exam is conducted in 13 different languages, namely, English, Hindi, Assamese, Bengali, Gujarati, Malayalam, Kannada, Marathi, Odia, Tamil, Telugu, Urdu, and Punjabi |
NEET Exam Section-wise Distribution:
In all 4 Subject sections, Physics, Chemistry, Biology, and Zoology, there are two sections, section A comprises 35 questions and section B comprises 15 questions out of which 10 are to be answered. Each question carries 4 marks.
Number of Seats for 2022-2023 at CMC, Vellore
The total number of MBBS candidate seats is 100 and the seat distribution is as follows:
- All India open category: 16 seats
a. One candidate is selected by Govt. of India under the ‘Central Pool Scheme’.
b. 20% i.e., 3 seats are reserved for the SC/ST candidates. - Minority Network Category & CMC, Vellore staff quota: 84 Seats
Steps to get admission into CMC Vellore
- Fill out the application form for an undergraduate course from the CMC, Vellore official site.
- Provide your NEET application form details.
- Submission of the receipts of the certification forms from Minority Network Organizations (if applicable).
- Apply to the Tamil Nadu Selection Committee for the counseling process in the relevant category.
- The selection is based on the NEET-UG score and candidates are required to fill the NEET-UG score and rank on the CMC, Vellore admission site.
- Submission of the Arno & rank of TN Management Quota.
- Be updated with the release of the merit list.
- Counseling by Tamil Nadu Selection Committee, DME, Chennai.
All these steps are to be done in the stipulated period as provided by the college. So, be updated.
Admission Process after Counseling at CMC, Vellore
- After the counseling procedure, the candidate is required to register for the course by paying the tuition fees and completing other formalities, and submitting original certificates.
- The admission confirmation is approved by Tamil Nadu Dr. M.G.R. Medical University. Until the approval, admission continues to be provisional.
- After the confirmation of the MBBS admission at CMC, Vellore, a candidate needs to submit their original required documents at the university campus.
- All the candidates getting admission to CMC, Vellore need to undergo a medical fitness check-up and the admission gets confirmed only after the medical fitness clearance by the Medical Board, CMC, Vellore.
MBBS Course Fee at CMC, Vellore
The fees to be paid at the time of registration for admissions to the MBBS course at CMC, Vellore is mentioned in the table below:
| Particulars | Fees (in rupees) |
| Tuition fees | 3,000 |
| One-time College fee at Admission | 10,300 |
| Other Annual Fee | 25,105 |
| One-time payment to the University | 14,425 |
| Total | 52,830 |
*The course fee may change in the coming years depending upon the University rules and regulations.
MBBS Cut-off at CMC, Vellore
Based upon the analysis of the previous years’ cut-offs, the estimated NEET-UG cut-off marks for the MBBS course for admission at CMC, Vellore are mentioned below:
| Category | Estimated Cut off Score |
| General | 600 |
| Minority | 380 |
| Institutional/Staff | 500 |
| SC/ST | 520 |
To get the conceptual clarity on the MBBS courses online, click here.
Medical Postgraduate Courses at CMC, Vellore
In CMC, Vellore Admission to PG Degree, Diploma, PG diploma courses, and fellowship courses come under the Group B category. Admission to the MD/MS courses is done based on the NEET-PG score. All the students need to get into the NEET-PG merit list for admission to the PG courses with the required cut-off score.
PG Courses and Number of Seats
The Christian Medical College offers admission to various post-graduate specialization courses.
- The CMC Vellore provides admission to MD courses for various subjects along with the number of seats mentioned below:
| MD Specialization Courses | Number of Seats |
| Anaesthesiology | 33 |
| Anatomy | 4 |
| Biochemistry | 2 |
| Community Medicine | 6 |
| Dermatology Venerol & Lep. | 5 |
| Emergency Medicine | 3 |
| Family Medicine | 2 |
| Geriatrics | 3 |
| General Medicine | 16 |
| Microbiology | 4 |
| Nuclear Medicine | 2 |
| Pediatrics | 20 |
| Pathology | 8 |
| Pharmacology | 2 |
| Physiology | 4 |
| Physical Medicine & Rehabilitation | 4 |
| Psychiatry | 12 |
| Radiodiagnosis | 12 |
| Radiation Oncology | 8 |
| Respiratory Medicine | 4 |
| Transfusion Medicine | 3 |
- The CMC Vellore provides admission to MS courses for various subjects along with the number of seats mentioned below:
| MS specialization Courses | Number of Seats |
| Otorhinolaryngology | 8 |
| General Surgery | 10 |
| Obstetrics & Gynecology | 17 |
| Ophthalmology | 9 |
| Orthopaedics | 12 |
Service Obligation at CMC, Vellore
- The service obligation of 3 years is mandated for all the MS/MD candidates, except for the clinical specialties (General merit category).
- Candidates admitted to the clinical specialties under the general merit category have a service obligation of 1 year.
- Candidates admitted to the pre-and para-clinical specialties under the general merit category, have no service obligation.
- For diploma courses, the service obligation period is a minimum of 2 years whereas, general merit candidates are exempted from the same.
- After the course completion, the service obligation is served at the CMC, Vellore or any of the associated mission hospitals.
Facilities available for the medical PG trainees
- Stipend
- Accommodation
- Research activity of each department
- Medical records department
- Recreation
- Staff/student health clinic
Fee Structure for the Postgraduate Medical Courses at CMC, Vellore
The fees to be paid at the time of registration for admissions to the Medical PG courses (MD/MS) at CMC are mentioned in the table below:
| Particulars | 2 yr Post Diploma Degree (in rupees) | 3 yr PG Degree (in rupees) |
| Tuition fees | 800 | 1200 |
| One-time admission fees | 1200 | 30,000 |
| University fees | 1,35,610 | 1,35,610 |
| Others | 17,600 | 19,600 |
| Total | 1,74,010 | 1,86,410 |
*The course fee may change in the coming years depending upon the University rules and regulations.
NEET-PG Cut-off Score for MS/MD admission to CMC, Vellore
Based upon the analysis of the previous years’ cut-offs, the estimated cut-off marks for the medical PG specialization courses for admission at CMC, Vellore are mentioned below:
| Specialization | Estimated Cut-off Score |
| Anesthesiology | 400 |
| Anatomy | 460 |
| Biochemistry | 430 |
| Community Medicine | 500 |
| Dip. In Clinical Pathology | 480 |
| Dermatology Venerol & Lep. | 540 |
| Emergency Medicine | 500 |
| Family Medicine | 450 |
| Geriatrics | 380 |
| General Surgery | 460 |
| General Medicine | 590 |
| Microbiology | 450 |
| Neurosurgery | 500 |
| Nuclear Medicine | 500 |
| Obstetrics & Gynecology | 380 |
| Ophthalmology | 400 |
| Orthopedics | 450 |
| Pediatrics | 440 |
| Pathology | 450 |
| Pharmacology | 600 |
| Physiology | 480 |
| Physical Medicine & Rehabilitation | 450 |
| Psychiatry | 360 |
| Radiodiagnosis | 450 |
| Radiation Oncology | 450 |
| Respiratory Medicine | 490 |
| Transfusion Medicine | 600 |
Certificate courses after MBBS
The certificate courses offered by the CMC Vellore for the MBBS graduates are mentioned below:
| Course Name | Duration | Number of Seats |
| Accident & Emergency Medicine | 2 years | 10 |
| Neonatology | 1 year | 1 |
| Palliative Medicine | 1 year | 2 |
| Acute Care Pediatrics | 1 year | 1 |
- CMC, Vellore also provides admission to various higher specialty and Postdoctoral diploma courses and allied health sciences courses.
- After completing MBBS, a medico can also pursue M.Sc. Epidemiology and Master of Public Health Administration.
CMC, Vellore Hostel Fees and Facility
- Hostel Facility for MBBS Students: MBBS students live in the campus hostels. The Bagayam campus of the CMC, Vellore has girls’ and boys’ hostels. The girls’ hostel is named as ‘Paradise on Earth’, while the boys’ hostel is named as ‘Mansion of the Gods’. Boys are required to submit the hostel charges (Deposits and advance) of10,000/- and girls Rs.8,000/-. The approximate living expenses per month for the hostel are Rs.6,000/- for boys and girls.
- Hostel facility for other courses: The women’s hostel and men’s hostel for the students of allied health courses are named as the ‘Fitch Hostel’ and the ‘Dorothy Joske Hostel’. The ‘Modale International Hostel’ is allocated for the elective course students/visitor observer students from overseas. The hostel and its charges vary as per the student’s course.
All the hostels are well equipped with all the necessities of a student and other facilities such as a Hostel Chapel, recreation room, gymnasium, library, dance room, music room, prayer room, mini kitchen, TV/Projector room. The food facility with vegetarian and non-vegetarian food is also available for all the residents.
How does DigiNerve help a medico?
DigiNerve is an EdTech initiative by Jaypee Brothers, a pioneer and market leader in health science publishing with a legacy spanning over 5 decades. It provides top-notch medical content to enhance conceptual clarity, clinical skills, and ace exams.
In terms of the calibre of the courses, the variety of subjects, the Gold Standard faculty, and the user-friendly interface, DigiNerve is unmatched.
- DigiNerve provides best online courses for MBBS subjects designed by eminent faculty as per CBME Curriculum and NEET Exam, such as
| MBBS Online Courses | Course Faculty |
| Community Medicine for UnderGrads | Dr. Bratati Banerjee |
| Forensics Medicine and Toxicology for UnderGrads | Dr. Gautam Biswas |
| Medicine for UnderGrads | Dr. Archith Boloor |
| Microbiology for UnderGrads | Dr. Apurba S Sastry, Dr. Sandhya Bhat, Dr. Deepashree R |
| OBGYN for UnderGrads | Dr. K Srinivas |
| Ophthalmology for UnderGrads | Dr. Parul Ichhpujani, Dr. Talvir Sidhu |
| Orthopaedics for UnderGrads | Dr. Vivek Pandey |
| Pathology for UnderGrads | Prof. Harsh Mohan, Prof. Ramadas Nayak, Dr. Debasis Gochhait |
| Pediatrics for UnderGrads | Dr. Santoah T Soans, Dr. Soundarya Mahalingam |
| Pharmacology for UnderGrads | Dr Sandeep Kaushal, Dr. Nirmal George |
| Surgery for UnderGrads | Dr. Sriram Bhat M |
- Apart from the MBBS and MD courses, DigiNerve brings the professional courses ‘Ultrasound in OBGYN Made Easy’ and ‘Basics of Infertility and IUI Made Easy’ by the top faculty Dr. Chaitanya Nagori and Dr. Sonal Panchal. After completion of the course, the candidates will earn a course completion certificate from Ian Donald Inter-University School of Medical Ultrasound.
- An Exam preparation course ‘Cracking MRCP Part 1’ by Dr. Gurpreet Singh Wander and Dr. Archith Boloor, helps a medico with their preparation to crack the MRCP exam. Cracking MRCP Part 1 course is based on the curriculum devised by The Royal College of Physicians (RCP). The course has 15 online modules covering major specialties such as Clinical Sciences, Cardiology, Gastroenterology, etc. The course includes video lectures, e-chapters, 2500+ BOF questions, mock exams, and most of all high-quality notes.
FAQs
-
How many marks are required in NEET for MBBS in CMC Vellore?
Ans: The estimated cut off score for admission to CMC, Vellore is around 600+ in the NEET Examination for general category. For the OBC/SC/ST & Minority groups, the estimated cut-off score is around 500 marks. For sponsored & management quota students, the cut-off range is comparatively lower.
-
Is CMC Vellore a deemed university?
Ans: No, CMC Vellore is not a deemed University. It is a private college, affiliated with Tamil Nadu Dr. M.G.R. Medical University, Chennai run by the Christian community.
-
Is CMC good for MBBS?
Ans: CMC Vellore is ranked 3rd as per NIRF ranking 2022 after AIIMS, Delhi, and PGIMER, Chandigarh. It is one of the best medical colleges in India.
Gynecology and obstetrics both focus on the female reproductive system. Gynecology deals with non-pregnant women whereas Obstetrics deals with pregnancy and the procedures and issues that go along with it, thus obstetrics deals with both the mother and the infant. To lower the risk of newborn disease and mortality, obstetricians closely collaborate with pediatricians and neonatologists on newborn care. They also remove cancers, fibroids, etc, surgically, although many gynecological problems require hormonal and other pharmacological therapy too.
What an obstetrician does:
The duties obstetricians carry out consist of:
- Obstetricians are in charge of collaborating with midwives to monitor and support a woman’s natural birth while she is in labor.
- One of their roles is to execute an episiotomy, which entails making precise cuts over the pregnant woman’s perineum to widen the birth canal.
- In some cases, assistance may be required to hasten protracted delivery to lessen maternal exhaustion and infant suffering (rising heart rate and possible brain damage to the baby). This makes use of methods like vacuum-assisted birth and forceps delivery.
- Caesarean (or C) section, calls for the baby to be surgically removed from the mother’s womb to lessen difficulties during labor. If a C-section is not used to hurry the delivery, difficulties could ultimately result in the baby’s death or physical harm.
- Therapy and diagnosis of ectopic pregnancy. When the fertilized ovum is implanted somewhere other than the womb, it results in an ectopic pregnancy. It frequently ends up in the fallopian tubes.
What a gynecologist does:
Gynecologists employ a variety of diagnostic and curative techniques. The following are a few of the common gynecological procedures:
- Hysterectomy or uterus removal
- Removing ovaries
- Fallopian tubes are removed during surgery
- Hysteroscopy and colposcopy involve employing tools like endoscopes to inspect the uterus’ inside.
- Taking care of uterine fibroids
- Identifying and treating sexually transmitted diseases
- Diagnosing menstrual issues, such as absence, severe bleeding, irregular or no periods, etc.
- Examination of the reproductive organs with ultrasound.
Objectives of Learning OBGYN
The Obstetrics and Gynecology Department offers modern, comprehensive screening and therapeutic techniques in a sympathetic environment for women in all stages of life.
In addition to regular gynecology procedures and medical treatments, a dedicated team provides cutting-edge motherhood facilities for routine and high-risk pregnancies, post-delivery and family planning services, sterility screening and handling, and all endoscopic gynecological operations.
Moreover, the department addresses high-risk pregnancies using prenatal diagnostic tests such as infant color doppler, amniocentesis, and velocimetry investigations. It also includes colposcopy, pap smear, and HPV-CO testing for going through menopausal women for cancer screening.
Aspirants can get a variety of profitable jobs in India and overseas by enrolling in this course. You can pursue additional education, such as research studies at prestigious universities and research institutions. Medical specialties like gynecology, cancer, critical care, reproductive endocrinology, or maternal-fetal medicine are all open to you as a career option. In India, postgraduate training in obstetrics and gynecology is either a three-year master’s program or a two-year diploma program. You can pursue a sub-specialty training program in fellowships after finishing your residency training.
OBGYN in MBBS
In their fourth year of MBBS, undergraduate students who are studying OBGYN participate in case discussions in the field of obstetrics and gynecology. A medico must also do a one-month OBGYN internship in addition to this. They receive instruction in the labor room, family planning OPD and OT, and obstetrics and gynecology OPD’s wards and OTs throughout their internship.
PG in OBGYN
A three-year, full-time postgraduate programme in OBGYN aims at training students to provide care to each patient, both pregnant and non-pregnant, as well as a thorough superior assessment of the entire medical pathology associated with the female reproductive organs.
Students learn about the most recent society standards, benchmark studies, breakthroughs in PCOS, robotic surgery, and conducting clinical examinations in OBGYN MD course. In the specialty clinics, OPD, wards, labour rooms, and operating rooms, they perform the necessary tests, interpret the results, and carry out medical/surgical management. They are taught to assess pregnancy-related issues using medical skills, find solutions, and provide pertinent prognoses.
Watch this video to learn the right way to approach OBGYN MD
Ph.D. Scholars of OBGYN
Every Ph.D. candidate has the privilege of choosing their specialty area from a list that includes fetal development and growth, hereditary and genomics, gestational diabetes, parental hepatitis, preeclampsia, prenatal analysis, and screening. Additionally, topics like urogynecology, endometriosis, endometrium, and establishment, prenatal cancer, and genital level are also discussed.
List of Top 10 Colleges for OBGYN in India
Here is the most recent list of top obstetrics and gynecology colleges in India that have earned official NMC recognition. These universities have the highest rankings and are even regarded as the most reputable universities in India
| S.No. | Name of College | Affiliation |
| 1 | Maulana Azad Medical College, Delhi | Delhi University |
| 2 | Kasturba Medical College, Mangalore | Manipal Academy of Higher Education (Deemed University), Manipal |
| 3 | Jawaharlal Institute Of Postgraduate Medical Education And Research (JIPMER), Pondicherry | Pondicherry University |
| 4 | Christian Medical College, Vellore | The Tamilnadu Dr. MGR Medical University, Chennai |
| 5 | Institute of Medical Sciences, Varanasi, Uttar Pradesh | Banaras Hindu University, Varanasi |
| 6 | Kasturba Medical College, Manipal | Manipal Academy of Higher Education (Deemed University), Manipal |
| 7 | Christian Medical College, Ludhiana | Baba Farid University of Health Sciences, Faridkot |
| 8 | Sri Ramachandra Institute of Higher Education and Research, Chennai | Sri Ramachandra Institute of Higher Education & Research (Deemed to be University), Chennai |
| 9 | SRM Medical College Hospital and Research Centre, Kancheepuram | SRM Institute of Science & Technology, Chennai |
| 10 | Dr. DY Patil Medical College Pune | Dr. D Y Patil University (Deemed), Pimpri, Pune |
Top OBGYN course online for best guidance for NEET Exam preparation
There is a great opportunity in the medical sector, particularly for OBGYNs, as the need for healthcare professionals is on the rise. Below are a few reasons why you should consider pursuing a career in OBGYN.
- Rising demand for OBGYNs
The need for female OB/GYNs has grown dramatically over the past few years, despite the perception that the health care industry is dominated by men. Today, more women than ever before are asking to consult a female specialist. Talking to other women comes more easily to women, especially when discussing sexual or pregnancy difficulties. Additionally, since more than 70% of residents are now women, supply and demand favor female OBGYNs.
- Great Earnings
The field of Obstetrics and Gynecology holds a bright future and is one of the most prestigious. Gynecology is currently one of the most lucrative medical professions. It is possible to work in government organizations, clinics, private practices, and universities, as well as in the most prestigious hospitals in India. Additionally, the candidate could open a surgical clinic. Obstetrician/Gynecologist salary in India ranges from ₹10 Lakhs to ₹ 36 Lakhs. Salary estimates are based on 199 salaries received from Gynecologists, particularly from a large hospital network.
- Fulfillment at work
One of the reasons people have named OBGYN as the most fulfilling profession in the healthcare industry is because bringing new life into this world is indeed a great sight to behold. As an OBGYN, you’ll have the opportunity to be regularly involved in childbirth and assist new mothers in making decisions that will impact the health of the infant.Only a few OBGYNs specialize in high-risk pregnancies. Patients with preterm births, a history of miscarriages, or antenatal problems that could complicate childbirth are cared for by these specialists. You’ll also have the ability as an OBGYN to advance the industry by developing novel techniques and procedures that may one day be considered best practices.
- Jobs & Career
- Salary
In OBGYN, OB refers to Obstetrics or Obstetrician, a doctor who specializes in the care of women and their babies during pregnancy and childbirth. GYN stands for Gynecology or Gynecologist, a doctor who specializes in the diagnosis and treatment of female reproductive disorders. OBGYN is a branch of medicine that deals with the entire female reproductive health of pregnant as well as non-pregnant females.
OBGYNs diagnose and treat diseases of the female reproductive organs. They treat various other women’s health issues such as hormonal problems, menstruation issues, contraception, infertility, and reproductive tract infections. They also hold the responsibility of childbirth via normal delivery, cesarian sections, pregnancy complications, fetal signs, and growth and also help women with psychological distress and counseling.
ADMISSION PROCEDURE
The following steps are undertaken by students who aspire to become an OBGYN:
- From the beginning, aspirants must complete the senior secondary education with the PCB stream with at least 50% marks.
- Further, they should crack the NEET UG exam to get admission to medical college (Government/ Private).
- After obtaining an MBBS degree, they need to appear for the NEET- PG entrance examination.
- A good score in NEET-PG gives a push to admission to the medical college for the OBGYN PG course.
- Aspirants must complete a junior resident responsibility to gain a post-graduation degree.
- After the successful completion, they must obtain a license and become board certified.
ELIGIBILITY FOR BECOMING AN OBGYN DOCTOR
- Candidates should have completed an MBBS degree from a college/institution recognized by the Medical Council of India (MCI) with a minimum of 55% marks.
- They must have undergone the one-year compulsory internship after completing the course.
- Candidates must clear the NEET PG exam to be eligible for admission to recognized universities/colleges.
- For the general category, the candidate must obtain at least 50th percentile marks in NEET PG for admission to MD/MS courses. For SC, ST, and OBC, the minimum percentage requirement is the 40th
- For the candidate with benchmark disability specified under the Rights of Persons with Disability Act 2016, for the GEN-EWS and unreserved category 45th percentile is required. For, SC/ST/OBC-NCL candidates, the minimum marks shall be 40th
- In some cases, admission to post-graduate medical courses may also include a group discussion/personal interview after the entrance examination depending on the college.
- Final confirmation of admission depends on the cut-off marks and the counseling procedure.
OBGYN IN MBBS
MBBS (Bachelor of Medicine and Bachelor of Surgery) is an undergraduate medical sciences course with a duration of 5.5 years including an internship. Admission to the MBBS is solely based on an entrance examination. The NEET (UG) entrance examination is the only valid examination to get admission in MBBS in government or private medical colleges recognized by MCI (Medical Council of India). A student needs to get into the merit list and undergo the counseling procedure for admission to MBBS successfully.
After getting admission to medical college, a student needs to learn various subjects like microbiology, pathology, pharmacology, medicine, pediatrics, OBGYN, community medicine, surgery, and more.
Undergraduate students study OBGYN in their 4th prof, where they go through case discussions in Obstetrics and Gynecology. Along with this, a medico needs to complete a one-month OBGYN internship. During this internship, they get training in Obstetrics & Gynaecology OPD’s Wards and OTs, Labour Room, and Family Planning OPD and OT.
PG OBGYN AFTER MBBS
OBGYN is a three-year full-time postgraduate course in medical sciences. The course consists of a comprehensive, superior examination of the complete medical pathology related to the female reproductive organs, and provision of care to each non-pregnant and pregnant patient.
Admission to OBGYN MD is done through national-level entrance examinations like NEET-PG, and INI-CET. In PG OBGYN, students get familiar with the latest society guidelines, benchmark trials, and recent advancements in PCOS, Robotic Surgery, and performing clinical examinations. They are asked for pertinent tests, decipher the results, and implement medical/surgical management in the specialty clinics, OPD, wards, labor room, and operating rooms. They learn to use medical capabilities to evaluate troubles in pregnancy and discover techniques and relevant prognoses.
Watch this video to understand this important topic of OBGYN through case-based discussion
ENTRANCE EXAMINATIONS FOR PURSUING PG OBGYN
MBBS students need to undergo and crack the NEET-PG entrance examination for admission to medical college for PG OBGYN. The NEET (National Eligibility cum Entrance Test) is a national-level entrance examination for admission to pursue medical sciences; NEET UG for the undergraduate medical courses (MBBS, BDS, BAMS, BHMS), and NEET PG for the doctors to get admitted to various postgraduate courses (MD/MS) and diploma courses.
Admission for PG to government and private colleges depends on the ranking of the medicos in the NEET-PG entrance Examination. The examination body of NEET PG is the National Board of Examinations and further, the Directorate General of Health Services conducts the counselling and seat allotment process.
Institutes that are exempted from admission via the NEET PG exam are:
- AIIMSs
- PGIMER
- JIPMER
- NIMHANS
- SCTIMST
These institutes come under the INI (Institute of National Importance).
To get admission to INI (Institute of National Importance) institutions, medicos must get into the merit of the INI-CET (Institute of National Importance Combined Entrance Test).
INI- CET is a combined entrance examination to the INI institutes for PG courses in medical Sciences [MD, MS, DM (6 years), MCh (6 years), and MDS]
List of Participating INI Institutes for INI-CET:
- All India Institute of Medical Sciences, New Delhi
- All India Institute of Medical Sciences, Bathinda, Punjab
- All India Institute of Medical Sciences, Bhopal, Madhya Pradesh
- All India Institute of Medical Sciences, Bhubaneswar, Odisha
- All India Institute of Medical Sciences, Bibinagar, Telangana
- All India Institute of Medical Sciences, Deoghar, Jharkhand
- All India Institute of Medical Sciences, Jodhpur, Rajasthan
- All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh
- All India Institute of Medical Sciences, Nagpur, Maharashtra
- All India Institute of Medical Sciences, Patna, Bihar
- All India Institute of Medical Sciences, Raipur, Chhattisgarh
- All India Institute of Medical Sciences, Rishikesh, Uttarakhand
- Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry
- Postgraduate Institute of Medical Science and Research (PGIMER), Chandigarh
- National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore, Karnataka
- Sree Chitra Tirunal Institute of Medical Sciences and Technology (SCTIMST), Thiruvananathapuram, Kerala
NOTE:
MRCOG Examination:
This examination is specially designed by the Royal College of Obstetricians and Gynaecologists for OBGYN doctors to assess their skills, knowledge, and competencies. This exam comprises three parts- MRCOG Part 1, MRCOG Part 2 & MRCOG Part 3. Membership of RCOGs is awarded upon the successful completion of all three stages of the exam.
TOP COLLEGES FOR PG IN OBGYN
Some of the colleges for admission to PG-OBGYN are listed below:
- All India Institute of Medical Sciences, New Delhi
- Armed Forces Medical College, Pune
- IMS BHU- Indian Institute of Medical Sciences- Banaras Hindu University, Banaras
- Bangalore Medical College, Bangalore
- Maulana Azad Medical College, New Delhi
- Lady Hardinge Medical College, New Delhi
- JIPMER (Jawaharlal Institute of Postgraduate Medical Education and Research), Puducherry
- Government Medical College and Hospital, Chandigarh
- King George Medical College, Lucknow
- Madras Medical College, Chennai
- Christian Medical College, Vellore, Tamil Nadu
- Maulana Azad Medical College, New Delhi
- VMMC College, New Delhi
- Goa Medical College, Panaji
COURSE STRUCTURE OF PG OBGYN
There are four papers:
PAPER I: Applied Basic sciences: Physiology and anatomy of the female reproductive system, pharmacological and hormonal roles, obstetric and gynecological markers – non-neoplastic and neoplastic, medical genetics, anatomical and physiological changes in the female reproductive tract during pregnancy, pharmacology of drugs used during labor and after birth
PAPER II: Obstetrics including Social Obstetrics & Diseases of Newborn: Prenatal Care: Risky Pregnancy, Obstetrics: Postpartum, Vaginal delivery, caesarean section, Hysterectomy, Destructive Surgery, Manipulation (external/internal pod version, manual placental removal, etc.), Medical Abortion – Safe Abortion – Case Selection, Complication Techniques, and Treatment, MTP, newborn.
PAPER Ill: Gynecology: Clinical gynecology, Family Welfare, and demography, Male and female infertility.
PAPER IV: Recent Advances in Obstetrics & Gynaecology
- Along with four theory papers, doctors pursuing MD OBGYN have to do Practical Examinations in Obstetrics and Gynecology:
Clinical long case and short case including viva of:
- Instruments
- Pathological specimen,
- Medicines and X-rays, ultrasounds, etc.
- Dummy Pelvis
- Family planning
THESIS: - Students identify relevant research questions
- Conduct a critical literature review
- Hypothesize
- Determine the most appropriate study design
- State the purpose of the research
- Preparation of test protocols
- Conduct the study according to the protocol
- Analyze and interpret research data and draw conclusions
- Write a research paper
- PG OBGYN students are also required to complete their OBGYN residency and postings.
Watch this video to learn the right way to approach OBGYN MD
SCOPE/JOB OPPORTUNITIES AFTER MD IN GYNECOLOGY & OBSTETRICS
Undoubtedly, the course is highly respected, job oriented, and lucrative. This opens doors to a variety of job prospects such as Maternal-fetal medicine specialists, Reproductive endocrinologists, Gynecologic oncologists, Female pelvic specialists, critical care medicine specialists, professors, clinical associates, junior consultants, senior residents, consultants, general physicians, researchers, private practitioners, govt. doctors, and private clinicians. Moreover, the OBGYN can go for research and higher studies in research centres and universities.
FAQs (Frequently asked questions)
Q1.What is the difference between an Obstetrician and a Gynecologist?
Ans. A gynecologist is mainly trained in female reproductive care whereas an obstetrician cares for pregnant women and newborns.
Q2. Who is the first female Surgeon General in India?
Ans. Mary Poonen Lukose was an Indian gynecologist, obstetrician, and the first female Surgeon General in India.
Q3. Can a person pursue OBGYN without an MBBS degree?
Ans. Yes, one can pursue a career in OBGYN after a BAMS degree if not MBBS. A diploma course in OBGYN can be done as well after a BAMS degree.
Q4. How can I enter the OBGYN field?
Ans. You can undergo a three-year postgraduate course in OBGYN (MS/MD) after doing MBBS or a two-year diploma program of postgraduate training in Obstetrics and gynecology.
COVID-19 has devastated families, institutions, and livelihoods while also scarring those at the front lines who witness it every single day. The strain put on our mental health during COVID-19 cannot be understated and the lockdown spent watching the news during such a time of extreme crisis has pressured our mental health further. It can be helpful to take moments out of your day to truly reflect on COVID-19’s impact on education and the mental health of students that might be fractured at the moment.
For those looking to pursue medicine, seeing crippling amounts of pressure being put on the healthcare system might be personally worrying. However, it is especially important to consider the mental health of students at such a critical juncture. To help take care of your mental health during covid-19, keep the following tips in mind to reduce stress.
- Free Headspace Subscription – Headspace is a US-based meditation app that announced a free subscription to all healthcare workers in India to tackle their mental health during COVID-19. Headspace has conducted numerous studies to reach the definitive conclusion that with just 30 days of guided meditation and practicing mindfulness, there has been a 30% stress reduction, greatly boosting mental health of students during COVID-19. If you are searching for a sense of peace in your days, consider signing up for Headspace.
- Take Care of Your Health – It can be difficult to separate your own life from those you care for but finding time to ensure that you are getting the exercise and nutrition you need is essential for myriad reasons. Firstly, an adequate diet that is supplemented with vitamins and nutritious food is essential to building up your immune system, an important factor when amid a pandemic. Secondly, as physical and mental health during covid-19 are interrelated, exercise regularly, try and sleep for full 8 hours, and eat healthy.
- Communicate Often – One of the best ways to destress and find a connection in an isolating time is to talk to other people. Be it friends, family, or a counselor, consider finding a connection and a way to unwind. Especially when considering COVID-19’s impact on the education and mental health of students during covid-19, these forms of socialization may provide a much-needed respite.
- Limit News – The endlessness of social media coupled with the stress of news can seriously harm the mental health of students during covid-19 and adults alike. While we all must remain alert about further developments in the pandemic, limit the amount of time that you ingest news.
If you find moments of solace through submerging yourself into challenging but rewarding tasks, perhaps signing up for an online course is a good way to spend your day. To get started, click here to view DigiNerve’s medical course options.
The Membership of the Royal Colleges of Physicians (MRCP) is a postgraduate medical degree by the United Kingdom that can be obtained through a three-part medical entrance exam. Being highly competitive, acing it requires mentoring and study guides. The MRCP exam has much allure, including prestige, international recognition, and boosting your CV but first students need to understand the basics of what the MRCP exam is, and what the three parts entail-
MRCP Part 1 – MRCP Part 1 is a written exam that involves two papers, each one is 3 hours long and contains 100 best of fives (BOF) questions. To crack the MRCP Part 1, detailed and consistent preparation is the key to the first attempt of success.
MRCP Part 2 (Written Exam) – The Part 2 course follows the same format as the MRCP part 1 exam structure and cracking it will take the same sincere preparation.
MRCP Part 2 (Clinical Paces Exam) – The clinical paces course is the last part of the MRCP exam and is the practical assessment of critical examination skills. It is conducted by two senior physicians as independent examiners who will observe and evaluate each student’s practical skills.
Now that you know the basic format of the MRCP exam, the question needs to be asked – why should you choose an MRCP degree?
- Recognition Abroad – While India recognises the MRCP degree as being equivalent to other postgraduate degrees, it has even more benefits if you plan to work outside of India. Due to its wide recognition and prestige, an MRCP degree holder has a significant advantage over other medical degrees, especially in other foreign countries like Australia, Ireland, Singapore, and various Gulf countries. With the status attached to an MRCP degree, you can get better job offers, more professional benefits, and higher pay. Lastly, successfully passing the MRCP exam boosts your CV for fellowships and other medical ventures. And these benefits alone make this postgraduate degree worth it!
- Gold Standard in Medical Qualification – The MRCP exam holds prestige because of its exclusivity, making it the gold standard in types of medical qualifications. It is also mentored by the acclaimed Dr. Gurpreet Singh Wander and Dr. ArchitBoloor, both of whom have published several books and are experts in the field. Further, the MRCP exam is run by the Federation of the Medical Royal Colleges in the UK, an exclusive set of colleges that are recognised as the best in medicine. All of these factors put MRCP degree holders at the top of their field that makes it the best choice for you.
- Worldwide Symbol of Excellence – Holders of the MRCP degree can subscribe to any or all three UK Royal Colleges of Physicians, boosting their professional status and putting the MRCP exam at the top of postgraduate courses. Further, the double benefit of being able to use an MRCP degree in India and various international countries gives you wider recognition and opens more career paths in the future.
- Improves Medical Knowledge and Boosts Skill – Because of the break up into part 1 and part 2 courses of the MRCP exam, the candidate receives better medical qualifications. The paces course encourages critical thinking that mimics the qualities needed as a working doctor and thus, puts the MRCP exam at advantage over other postgraduate medical entrances. Further, to prepare extensively for the part 1 exam, Diginerveprovides a thorough course, ‘Cracking MRCP Part-1’ that consists of live webinars, video lectures, detailed course modules, and 3000 practice questions, all of which ensures improved skill and knowledge.
- Shortest Way to a Successful Medical Career – The MRCP degree is now regarded as the quickest method of reaching a successful and international medical career. The MRCP exam structure and preparation with the ‘Cracking MRCP Part-1’ course has been designed to ensure that students have the basic skills and knowledge needed in their careers. Further, being highly prepared in the first attempt ultimately leads to a shorter training time for the entire exam in comparison to other postgraduate courses.
Now that you have a basic understanding of what an MRCP degree is and how the ‘Cracking MRCP Part-1’ course can help you ace it, you can start planning for the exam. Get your MRCP books ready, find the exam date that works for you, manage the fees, and prepare to ace the MRCP exam to start your successful career as a doctor. Lastly, when you take the course with DigiNerve, you get an exclusive bank of practice questions, personal mentor support, and detailed course manuals, all of which make your preparation a smooth journey. To get started, click here.
Every medical student knows that the MRCP exam is one of the most prestigious postgraduate medical courses and allows graduates to practice medicine in India and worldwide, including Asian, European, and Gulf countries. Originally from the UK and conducted by the Royal Colleges of Physicians, the MRCP exam has two parts – part 1 and part 2 course. Part 1 is a written exam consisting of two papers, 100 best of five questions (BOF), and a time limit of 3 hours, all of which make cracking the MRCP exam very difficult. However, there are several advantages to passing the MRCP exam. Apart from being able to practice medicine in countries like Australia, Ireland, and Singapore, it also boosts your CV because of its global prestige. If you do want the wider recognition that passing the MRCP exam ensures, to get started, here are a few things to know about eligibility for an MRCP degree:
- Existing Medical Degree – The MRCP exam is for postgraduates which means that you need to obtain a bachelor’s degree before you can consider attempting it. Further, you can only apply to take the MRCP exam a minimum of one year after you have completed your medical graduation and this precious time should be spent sincerely studying for this notoriously competitive exam.
- Years of Medical Training – To apply for the MRCP exam, you need to have completed a minimum of one year of medical employment. This includes internships and other fellowships during which you have successfully gained practical medical knowledge that you will later require for the paces exam of the MRCP. To make the process easier, ensure that you have already completed your required medical employment so that you can focus on MRCP preparation.
- The Number of Attempts Allowed – The MRCP exam has a limit to the number of attempts allowed – you can attempt the MRCP medical entrance exam a maximum of six times each. Thus, you can appear for part 1 and part 2 six times each. However, you must clear part 2 and the paces course within 7 years of completing part 1. To set yourself on the right track and prevent excessive attempts, good preparation for the first attempt is the key to MRCP success. You can achieve this by rigorously using the material provided in the ‘Cracking MRCP Part-1’, a detailed MRCP preparatory course offered on DigiNerve, and guided by India’s top faculty- Dr. Gurpreet Singh Wander and Dr. Archith Boloor.
- Exam Dates and Application Process – Once you’ve studied enough and are ready to attempt the MRCP exam, you need to book an exam date. The MRCP part 1 exam dates are set three times a year, in January, May, and September, with applications opening three months before each exam date. Once you have completed your preparation with ‘Cracking MRCP Part-1’, you can apply for the exam by registering through the official Royal Colleges of the UK website.
- Fees and Age Limit – To be eligible for the MRCP exam, a fee of £594 for international applicants, and £419 for UK applicants are required. Luckily, there is no age bar imposed to appear for the MRCP exam as it is open to all students who have sufficiently prepared.
Despite being highly competitive, acing the MRCP exam is easy with expert guidance, like the acclaimed Dr. Gurpreet Singh Wander and Dr. Archith Boloor, and with a focused study plan, complete with extensive course material on an accessible platform like DigiNerve. Now that you are informed of the eligibility criteria for the MRCP exams, know that the ‘Cracking MRCP Part-1’ is the key to success. By providing students with video lectures, over 3000 BOF questions, mock tests, and mentor support, every student will have the tools needed to crack the MRCP exam. To begin your exam preparation journey, click here to get started with DigiNerve.
DigiNerve is an online medical education platform by Jaypee Brothers, and it is here to solve all the tutoring needs of medical undergraduate students, postgraduate students, and professionals. It aims to provide top-notch content to improve concept-building, acquire clinical skills, and crack exams by top-class faculty, accessible anytime, anywhere.
There are four categories of courses offered by DigiNerve: UnderGrad, PostGrad, Professional, and Exam Prep.
UnderGrad Category includes courses for 2nd, 3rd, and 4th year MBBS subjects:
- Microbiology for UnderGrads by Dr. Apurba S Sastry, Dr. Sandhya Bhat & Dr. Deepashree R
- Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait
- Pharmacology for UnderGrads by Dr. Sandeep Kaushal & Dr. Nirmal George
- Forensic Medicine and Toxicology for UnderGrads by Dr. Gautam Biswas
- Ophthalmology for UnderGrads by Dr. Parul Ichhpujani & Dr. Talvir Sidhu
- Community Medicine for UnderGrads by Dr. Bratati Banerjee
- Pediatrics for UnderGrads by Dr. Santosh T Soans & Dr. Soundarya Mahalingam
- Orthopaedics for UnderGrads by Dr. Vivek Pandey
- Medicine for UnderGrads by Dr. Archith Boloor
- Surgery for UnderGrads by Dr. Sriram Bhat M
- OBGYN for UnderGrads by Dr. K Srinivas
Additionally, two combos are also available in the UnderGrads section,
- Basic Sciences Combo: This combo includes the second professional courses (Microbiology, Pathology, and Pharmacology) along with Clinics to provide them a clinical foundation in 2nd prof.
- Clinical Combo: This combo includes Medicine, Surgery, OBGYN, Orthopaedics, Ophthalmology, Community Medicine, Pediatrics and Forensic Medicine & Toxicology course.
PostGrad Category includes PG specialisation courses:
- OBGYN MD by Dr. Aswath Kumar
- Dermatology MD by Dr. Rashmi Sarkar & Dr. S. Sacchidanand
- Ophthalmology MD by Dr. N. Venkatesh Prajna
- Pediatrics MD by Prof. Piyush Gupta
- Medicine MD by Dr. Jyotirmoy Pal and Dr. Shashank R Joshi
- Surgery MS by Prof. (Dr.) Nilay Mandal
Professional Category includes the following courses:
- Ultrasound in OBGYN Made Easy by Dr. Sonal Panchal & Dr. Chaitanya Nagori
- Basics of Infertility & IUI Made Easy by Dr. Chaitanya Nagori & Dr. Sonal Panchal
- Ganga Videos on Spine Surgery by Prof. Rajasekaran Shanmuganathan, Dr. Ajoy Prasad Shetty & Dr. Rishi Mukesh Kanna
- Advance Course in Ultrasound and Infertility by Dr. Sonal Panchal and Dr. Chaitanya Nagori
- Critical Care Simplified by Dr. Yatin Mehta, Dr. Subhal Dixit, and Dr. Kapil G. Zirpe
- Organ Donation Simplified by Dr. Kapil G. Zirpe and Dr. Rahul Pandit
- Cosmetic Botulinum Toxin Simplified by Dr. Rasya Dixit, Dr. Urmila Nischal and Dr. K.C. Nischal
Exam Prep Category includes the following courses:
- Cracking MRCOG Part 1- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 1- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 2- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 2- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 3- Live OSCEs Engagement by Dr. Richa Saxena
- Cracking MRCOG Part 3- Non-Interactive OSCEs by Dr. Richa Saxena
- Cracking MRCP Part 1 by Dr. Gurpreet Singh Wander and Dr. Archith Boloor
Why Choose DigiNerve?
The course content offered by DigiNerve is not only as per the respective curriculums but is also brought to students easily and interactively. The courses include highly illustrative video lectures, competitive self-assessment questions, progress analysis, and specially curated notes while always focusing on concept-based learning. Here are a few other aspects of DigiNerve that set it as the best guide a student can have during their Top Doc journey:
- Esteemed Faculty: Each course on DigiNerve is curated and taught by Gold Standard Faculty in the respective field. For example, ‘Cracking MRCP Part-1’ is taught by the highly acclaimed Dr. Gurpreet Singh Wander and Dr. Archith Boloor, each of whom has published research papers and taught at renowned medical universities. Similarly, ‘Ultrasound in OBGYN Made Easy’ is structured and mentored by the distinguished faculty, Dr. Sonal Panchal and Dr. Chaitanya Nagori, who have years of expertise and have published successful books on gynecology. Also, UG courses such as Microbiology for UnderGrads is taught by the maestro himself, Dr. Apurba S Sastry along with Dr. Sandhya Bhat & Dr. Deepashree R, Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait. These faculties already have an irreplaceable place on the shelves of every medical student. Thus, all students can be assured that no matter which course they choose, DigiNerve has got their back.
- Credible Content: Since all course content is structured by renowned faculty, all students get the latest medical breakthroughs, practically relevant material, clinical case demonstrations & discussions, and the benefit of over 50-year trusted medical legacy that Jaypee provides. All of this results in courses that have credible and valuable information to help students not only ace their medical and entrance exams but also develop their professional abilities as doctors.
- Easy to Use: DigiNerve is designed to be as student-friendly as possible. With an efficient and detailed website and a virtual classroom experience that is based on interactivity, all students can access courses and navigate with ease. Further, students can learn from their respective courses and content anytime and anywhere via the DigiNerve App. The app also has other great features, such as the Continue Journey Widget, Split View option to access the video lectures and notes simultaneously, Video Indexing, and ‘Ask a doubt’ feature.
- Specialization Courses: Apart from providing students with courses to help them crack competitive exams, DigiNerve also has specialized courses for doctors looking to hone in on a particular skill or for postgraduate students looking to enhance their practical knowledge. One such course is ‘Ultrasound in OBGYN Made Easy’. The course provides students with detailed knowledge of ultrasounds that is essential for gynecology and radiology practice. It also specifically teaches cutting-edge fetal medicine knowledge to help doctors reach a diagnosis.
- International Certification: On completion of the specialized courses offered in Infertility and IUI and Ultrasound in OBGYN, DigiNerve facilitates internationally recognized certificates for its students. Thus, boosting their CV, opening doors for higher pay and international practice in the respective specialization. For some courses like the USG course, students on completion receive a certificate from the prestigious Ian Donald Inter-University School.
DigiNerve is unparalleled in the quality of courses offered, the range of material taught, the Gold Standard faculty that structure and teach the courses, and the easily navigable interface. Thus, giving students helpful courses at a competitive price that provide them with conceptual clarity, allowing them to excel in their exams, and also offering practical guidance.
Ultrasound in OBGYN Made Easy is an in-depth course that has been structured to ensure focus on the clinical application of academic knowledge that will help hone gynecology skills. The Ultrasound in OBGYN Made Easy course is structured and mentored by the renowned Dr. Sonal Panchal and Dr. Chaitanya Nagori to ensure the highest quality of ultrasound education for all obstetricians and gynecologists looking to do ultrasounds for their own patients, or for radiologists who need to master gynecological and obstetric scans. At the end of the course, and on completing the certification exam, students will be awarded an internationally recognized certificate from Ian Donald University for their ultrasound skills. Thus, ‘Ultrasound in OBGYN Made Easy’ is a must for all obstetricians and gynecologists who need to master the application of ultrasound in their routine practice. But why is this course worth it? Here are the reasons why this course is essential for all practitioners who need to excel in the art of ultrasound:
- Strong Foundation – With pioneer instructors, excellent lectures, and detailed notes in ultrasound, this course is the best way to build the foundations needed to start an independent clinic by teaching students the basics of ultrasound. By including all practical points and combining case demonstrations with video lectures, ‘Ultrasound in OBGYN Made Easy’ is the most efficient way to develop ultrasound skills that are essential in the fields of gynecology and radiology. Further, the course covers 11 topics that have been carefully structured to give students premium ultrasound knowledge.
- Highly Acclaimed Instructors – This stellar ultrasound course has extremely prestigious faculty attached to it, Dr. Sonal Panchal has more than twenty years’ worth of field experience as a consultant radiologist and also specializes in ultrasound in obstetrics and gynecology. Similarly, Dr. Chaitanya Nagori is the Director of Dr. Nagori’s Institute of Infertility and has published several books on Obstetrics and Gynecology. With these instructors at the helm, students are guaranteed expert education that can easily be applied in their practices.
- Prestigious Certification – On completing the ‘Ultrasound in OBGYN Made Easy’ certification exam, students will be awarded an internationally recognized certificate from the Ian Donald Inter-University School of Medical Ultrasound. This distinguishment will set their practice apart greatly and will further their gynecology and obstetrics as well as provide the confidence they need to excel in their fields.
- Fetal Medicine Knowledge – Fetal medicine is a growing specialty that requires inspection by radiologists and obstetricians specifically to distinguish between normal and abnormal ultrasound scans. This specialization is exactly what will be taught in great detail, and with care in this course. By the end, students will learn all the practical points to be able to correctly diagnose these issues.
- Provides Required Ultrasound Knowledge – Confidence in conducting ultrasounds is needed by all doctors to be able to diagnose accurately and the ‘Ultrasound in OBGYN Made Easy’ course will give them exactly that. The course has been constructed to provide doctors with pro-tips for diagnosing fetal abnormalities in ultrasounds, along with other patients with gynecological complaints. Due to this specialization, and through 8 hours of video lectures along with class demonstrations, hundreds of pages of notes, and 100 MCQs, students can complete the course with a newfound confidence in their ultrasound diagnostic skills. On top of that, these skills are being taught by highly specialized faculty that will ensure that all students learn the required knowledge for ultrasounds.
Now that you know the basics of the ‘Ultrasound in OBGYN Made Easy’ course and the various methods employed to increase the confidence of all practitioners, here are a few important facts to know so that your journey can begin:
- Course Duration – This course will last for two months, during which 11 topics will be covered, and lecture videos, notes, and self-assessment questions will be distributed on the DigiNerve platform. At the end of the course, students will earn their certificate from the Ian Donald Inter-University School of Medical Ultrasound.
- Course Fee – This detailed and comprehensive ultrasound course, including tax, will cost Rs. 35,000 for which the students will receive all the material needed to give them the confidence and practical knowledge needed for practicing ultrasounds successfully.
Now that you have the information ready to make a decision, choose ‘Ultrasound in OBGYN Made Easy’ to give you the confidence and practical knowledge to ensure that you’re at the top of your field. The platform that this course is presented on, DigiNerve, is easy to understand, efficient, and is catered to every student’s needs. To enroll now, click here.
The MRCP Part 1 exam is your first step towards the very prestigious Royal College Membership. The exam is challenging, and students spend months preparing for it. You have to study while balancing work, recreation, and any other commitments you have going on, so it’s important to study smart. Here are some tips to prepare for the exam, so that you don’t spend crucial time trying to figure out what approach to take or what MRCP study materials to use.
Create a structured study plan
Familiarise yourself with the syllabus and estimate how much time each topic will take you depending on how fast you absorb the material. Allocate less time to topics you find easy or already know well, and more time to topics you find difficult or that require a more thorough understanding. Calculate the total time it will take you to study all of MRCP study material against the time you can spend studying in the upcoming months as well. Use your plan to stay on track with studying.
Find comprehensive course material
Online courses such as Diginerve’s Cracking MRCP Part 1 are the best comprehensive study material, as in one course, you get mentorship and webinars from distinguished faculty, a comprehensive course manual, notes, practice questions, mock exams, and performance tracking.
Do practice questions
Practice a lot. Anyone who has passed the MRCP exam will tell you that the key to passing the MRCP medical exam is to do as many MRCP practice questions as you can. Practice questions truly test your knowledge as they force you to apply what you’ve learnt. Diginerve’s Cracking MRCP Part 1 also has thousands of practice MRCP questions, ideal for thorough revision and practice.
Simulate the exam
The MRCP part 1 exam has 200 multiple choice questions split between 2 papers, each of which is 3 hours long. You need to build up stamina to keep your brain from tiring out in the middle of the medical exam. To keep working at your optimum pace throughout the MRCP medical exam, put yourself in the exact same conditions that you’ll be in when you take the exam- don’t take any breaks or talk to anyone during it. You don’t want to be sitting in the real medical exam with your brain fried and your fingers tired. The Cracking MRCP Part 1 course offers several mock exams you can take to gauge how you are doing. You can score yourself using Cracking MRCP’s mock papers, and then see how you’re doing compared to your peers on the course’s online leaderboard.
Study with a group
You may feel stressed as you study for the MRCP part 1 exam while handling work and a busy schedule. Working with others who are appearing for the medical exam will keep you motivated and make you feel like you’re not alone. When you work in groups, ideas are shared and questions are solved together. If you don’t understand a question, your friend might be able to explain it to you, which will help both your understanding and theirs.
Cracking MRCP Part 1 course offers the facility of Forums where you could interact with fellow participants and learn from each other.
The MRCP exam is one of the toughest exams to pass – but at the end of it, you walk away with an internationally recognized qualification that makes all the hard work worth it. Your job and studies are probably keeping you busy already, so it is important that you optimize your time and study for the MRCP the smart way. Here are seven tips on how to crack the MRCP Exam:
1. Stay focused on the exams
You want to allocate at least a few hours a day to MRCP exam preparation, as consistency is important. You don’t need to spend all day on the MRCP study material. Focused studying for a few hours everyday is the key to success.
2. Practice answering questions
The most important MRCP test preparation you can do is to get yourself a book of practice questions to ensure you understand the format of the test and recognize patterns in the questions. You can also try an MRCP questions bank, with Cracking MRCP Part 1, for practice.
3. Cover all the specialties in the curriculum
Try solving as many questions from the range of specialties covered in the curriculum as you can, to ensure you have a thorough knowledge of each topic. Diginerve’s app has notes and questions on every topic you need to know.
4. Find reliable MRCP study material
Make sure your MRCP study material is detailed, thorough, and covers everything you need to know. Jaypee has course manuals, revision notes, and practice papers for MRCP part 1 and MRCP part 2, and an online course with mentorship, webinars, practice questions, mock papers case studies, and revision notes for MRCP Part 1.
5. Do mock exams under timed conditions.
The MRCP tests are a marathon, not a sprint. You need to be prepared to answer hundreds of questions. Mock papers by Cracking MRCP Part 1 help you test yourself and measure your progress against peers on a leaderboard.
6. Understand the concepts, don’t just memorize
When you practice, you also need to understand the reasoning behind why an answer is wrong or right. If you only memorize, you might find yourself confused in the actual MRCP exam. Understanding the concepts will give you a better understanding and make you a better doctor overall.
7. Ask people who’ve passed the MRCP for advice
You probably know doctors who have passed the MRCP part 1 and MRCP part 2 and attained the MRCP degree. Ask them what to do and how to study. Whatever methods they used, they passed, so approaching the test in a similar way means you’re on the right track.