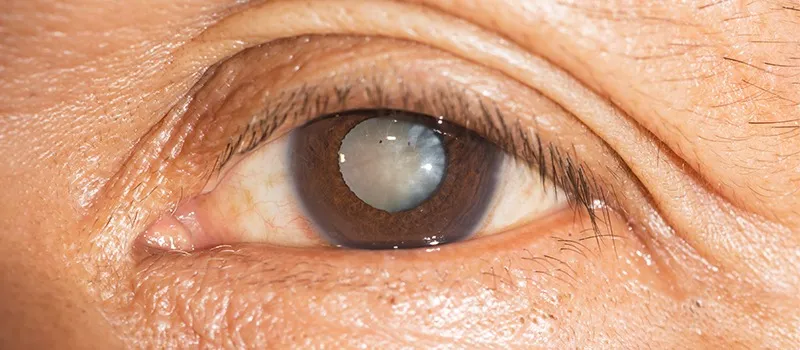
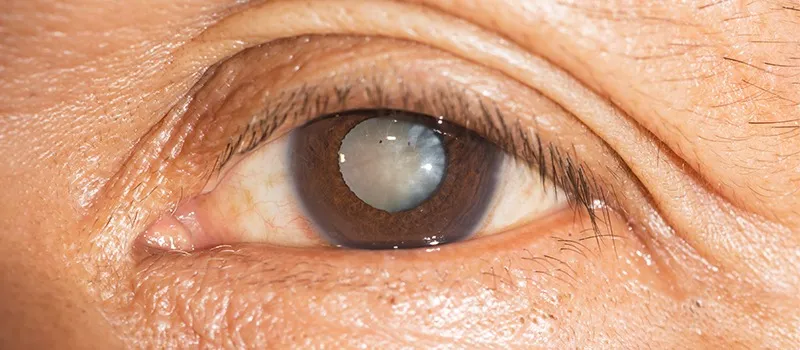
How to Manage a Senile Cataract Patient?
A cataract is referred to as the development of any opacity in the lens or its capsule. It may occur either due to the formation of opaque lens fibers (congenital and developmental cataracts) or due to a degenerative process leading to the opacification of normally formed lens fibers (acquired cataracts).
Classification:
The Etiological Classification includes the following types of cataracts:
- Congenital and Developmental Cataract
- Acquired Cataract
- Senile cataract
- Traumatic cataract
- Cataracts in systemic diseases
- Electric cataract
- Radiational cataract
- Toxic cataract
The Morphological Classification includes the following types of cataracts:
- Capsular Cataract
- Subcapsular Cataract
- Cortical Cataract
- Nuclear Cataract
- Polar Cataract
SENILE CATARACT
Senile cataract is also known as Age-related cataract and is the most common type of acquired cataract. It affects equally all persons of either sex above the age of 50 years. The condition is usually bilateral, but in most cases, one eye is affected before the other.
ETIOLOGY
Some of the risk factors associated with Senile cataracts:
- Age: It is the most important factor.
- Sex: Its prevalence is greater in females.
- Heredity
- Ultraviolet Irradiations: It is responsible for the early onset and early maturation of senile cataracts.
- Dietary factors: Diet deficiency in certain proteins, amino acids, and vitamins (riboflavin, vitamin A, C, E).
- Dehydration Crisis
- Smoking: When a person smokes, it leads to the accumulation of pigmented molecules like 3-hydroxykynurenine and chromophores, which lead to the yellowing of the lens.
HOW LENS LOSES ITS TRANSPARENCY?
Lens gets affected in different ways in nuclear and cortical senile cataracts. In cortical cataracts, there is a decrease in the soluble crystalline lens proteins, amino acids, and potassium associated with an increase in the concentration of sodium, which ultimately results in over hydration of the lens. While in nuclear cataracts, there is age-related nuclear sclerosis associated with dehydration and compaction of the lens. It is associated with an increase in water-insoluble proteins.
STAGES OF MATURATION
- In-nuclear type of Cataract
The sclerotic process continues and leads to the hardening of the lens and decreases the ability of accommodation. The changes start from the centre and spread towards the periphery slowly.
- In-cortical type of cataract
Firstly, there is a stage of lamellar separation which is the earliest sign where the formation of vacuoles occurs in the cortex. These changes are reversible. It is followed by a stage of an incipient cataract where wedge-shaped or saucer-shaped opacity is seen. Then comes the final three stages of cataracts: immature, mature, and hyper mature (morgagnian and sclerotic) cataracts.
CLINICAL FEATURES
The clinical features include the symptoms, signs, and complications.
Symptoms:
- Glare
- Uniocular diplopia
- Colored halos around light
- Poor colored discrimination
- Black spots in front of the eye
- Image blur and misty vision
- Deterioration of vision
Signs:
- Visual acuity: It is 6/9 to PL+ and PR in all quadrants
- Test for iris shadow: It is seen in immature cataracts.
- Colour of lens:
- In nuclear cataracts: amber, brown, black, reddish
- In immature senile cataract: greyish white
- In mature senile cataract: pearly white
- In morgagnian hyper mature cataract: milky white
- In sclerotic hyper mature cataract: dirty white
- Morphology of lens: It is best seen by slit lamp examination.
- Distant direct ophthalmoscopy:
- Absence of opacity: reddish yellow fundal glow observed
- Partial cataractous: black shadow against the red glow observed
- Complete cataractous: no red glow observed
Complications:
- Phacoanaphylactic uveitis
- Lens-induced glaucoma
- Subluxation or dislocation of the lens
Click here to watch the best online video lectures on lens and cataract.
MANAGEMENT OF CATARACT IN ADULTS
- NON-SURGICAL MANAGEMENT
To delay the progression of the disease:
- Vitamin E and aspirin can be taken
- Topical preparations containing iodide salts of calcium and potassium can be taken
-
- To treat the cause of cataract: control diabetes, remove cataractogenic drugs, removal of irradiations
- To improve vision in early stages of cataract: prescription of glasses, arrangement of illumination, use of dark goggles, and mydriatic agent.
- SURGICAL MANAGEMENT
Indications:
- Visual Improvement
- Medical Indications
- Cosmetic Indications
PREOPERATIVE EVALUATION AND WORKUP
1.) Ocular examination
It includes the following parameters:
- Visual status assessment
- Pupil
- Anterior segment evaluation
- Intraocular pressure
- Examination of lids, conjunctiva, and lacrimal apparatus
- Dilated fundus examination
- Retinal function tests
- B- scan ultrasonography
- Electrophysiological evaluation
- Keratometry, corneal topography, and biometry
2. General medical examination of the patient
The medical examination should include the following:
- History of current medication
- Any family history
- Investigations
3. Preoperative medications
The preoperative prescribed medication includes:
- Antibiotics
- IOP lowering agents
- Mydriatic agent
- Anaesthetic agents
4. Surgery
- Earlier, couching was done in which the cataractous lens was pushed into the vitreous cavity, and it was the first surgery introduced.
- Then, crude extracapsular cataract extraction was done but soon it became unpopular due to marked complications.
- Later, intracapsular cataract extraction was introduced but nowadays it is not performed due to complications. It is reserved only in cases of subluxated or dislocated lens.
- Now comes the modern technique of extracapsular cataract extraction, which is the preferred method in all cases of cataract surgeries.
OVERVIEW OF EXTRACAPSULAR CATARACT EXTRACTION SURGERY:
In this method, the anterior capsule’s major portion is removed along with the anterior epithelium, nucleus, and cortex leaving behind the intact posterior capsule.
Indications:
- For almost all types of cataract surgeries in adults and children unless contraindicated.
Contraindications:
- In the subluxated or dislocated lens.
Advantages :
- Universal operation
- Posterior chamber IOL can be implanted after ECCE
- Postoperative vitreous-related complications are not seen
- Incidences of postoperative complications are much less like endophthalmitis, cystoid macular edema, and retinal detachment.
- Postoperative astigmatism is less
- Incidence of secondary rubeosis in diabetics is reduced
Different Techniques of Extracapsular Cataract Extraction:
- Conventional extracapsular cataract extraction
- Manual small incision cataract surgery
- Phacoemulsification
- Femtosecond laser-assisted cataract surgery
Presently, the phacoemulsification technique has become the preferred method of cataract extraction worldwide because the complications are much lesser as compared to other methods of cataract extraction.
However, in countries like India, manual small incision cataract surgery has the advantages of sutureless surgery as well as a low-cost alternative to phacoemulsification.
SURGICAL TECHNIQUES FOR CHILDHOOD CATARACTS:
The surgical methods opted for the childhood cataracts, include:
- Lens aspiration
- Lensectomy
INTRAOCULAR LENS IMPLANTATION:
IOL is the method of choice for correcting aphakia.
Types Of IOLs:
- Based on the method of fixation in the eye, the different types of IOL are:
- Anterior chamber IOL
- Iris-supported lens
- Posterior chamber lenses
- Depending upon the material of manufacturing, the different types of IOL are:
- Rigid IOLs
- Foldable IOLs
- Thinner foldable IOLs
- Ultra-thin foldable IOLs
- Based on focusing abilities, the different types of IOL are:
- Monofocal IOLs
- Multifocal IOLs
- Trifocal IOLs
- Special function IOLs, the different types of IOL are:
- Aniridia IOLs
- Implantable miniature telescope
- Piggyback IOLs
- Spherical versus Toric IOLs
- Aphakic versus Phakic Refractive IOLs
Indications of IOL:
It is done in each and every case being operated for cataract unless and until it is contraindicated.
BIOMETRY is the calculation of IOL:
Nowadays online toric IOL power is calculated.
Equipment for Biometry:
- A-Scan Ultrasonic Biometer
- Optical Biometer
Techniques of IOL Implantation:
- Primary IOL Implantation refers to the use of IOL during any surgery for a cataract.
- Secondary IOL Implantation is done to correct aphakia in the previously operated eye.
POSTOPERATIVE MANAGEMENT FOLLOWING CATARACT SURGERY
- The patient is asked to sit leaned back on chair for 30 minutes.
- Any NSAIDs may be given orally for mild to moderate postoperative pain.
- The bandage or eye patch is applied till the next morning. The eye is inspected for any postoperative complications.
- Antibiotic eye drops are used 4 times a day for 7-10 days.
- Topical steroids eye drops are given 3 to 4 times a day and are taken for 6-8 weeks.
- Topical ketorolac or any other NSAIDs with eye drops are given 2 to 3 times a day for 4 weeks.
- Topical timolol eye drops
To get conceptual clarity in Ophthalmology online, subscribe to CBME & NEET-oriented Ophthalmology for UnderGrads course.
Frequently Asked Questions
-
What causes senile cataract?
Ans: Senile cataract etiopathogenesis is not exactly clear, but it is mainly due to the age factor. Other factors are also responsible like heredity, ultraviolet radiation, dietary factors, dehydration crisis, and smoking.
-
What is the most common type of senile cataract?
Ans: Nuclear sclerotic type is the most common of senile cataracts in which there is progressive sclerosis of the nucleus of the lens. It makes the lens inelastic and decreases the accommodation ability, which hampers the light rays to pass.
-
Is senile cataract curable?
Ans: Yes, senile cataract is curable. It can be treated through surgeries like extracapsular cataract extraction and intracapsular cataract extraction.
-
What happens if cataracts are left untreated?
Ans: If the cataracts are left untreated, they lead to various complications like phacoanaphylactic uveitis, lens-induced glaucoma, and subluxation or dislocation of the lens.
Related post
Related Courses
Pathology for UnderGrads
Prof Harsh Mohan , Prof Ramadas Nayak , Dr Debasis...
Microbiology for UnderGrads
Dr Apurba S Sastry , Dr Sandhya Bhat , Dr Deepashr...